Abstract
Introduction: Multi-disciplinary healthcare providers need to move beyond task-based responsibility towards a more collaborative approach. Chronic childhood diseases such as bronchial asthma demands effective multidisciplinary team collaboration to improve patient care. Objective: We aimed to examine the interprofessional collaboration between physicians and pharmacists in the management of paediatric bronchial asthm, to explore the views and experiences of both pharmacists and physicians on the important aspects of Paediatric Respiratory Medication Therapy Adherence Clinic (PRMTAC) and patient-centeredness, and to identify barriers against interprofessional shared decision-making in the management of paediatrics bronchial asthma. Method: The study involved a face-to-face interview involving paediatric medical officers and pharmacists involved with PRMTAC. The semi-structured interview included four pharmacists and three paediatric resident physicians from Hospital Tuanku Fauziah, Perlis, Malaysia. A full audio recording was used for detailed data retrieval and verbatim transcription. The session was deemed completed once all the probed questions had reached a thematic conclusion. Result and Discussion: Three main themes emerged: (I) The relevance and necessity of PRMTAC service to complement paediatric outpatient bronchial asthma management, (II) the lack of communication between pharmacist-physician in outpatient bronchial asthma management, and (III) recommendations for a combined clinic in the management of outpatient paediatric bronchial asthma. PRMTAC services were rated as highly relevant in the management of outpatient bronchial asthma among all study respondents, irrespective of profession. The detailed assessment of medication compliance and technical demonstration provided by PRMTAC services were deemed fundamental in holistic patient care. The current clinical scenario demonstrates that the pharmacist and paediatric medical team work independently and in parallel, rather than collaboratively. Such workflow challenges in-tandem decision-making with regards to patient-focused medication. The lack of interaction also impedes sharing of ideas and new knowledge that could benefit both parties in relation to the management of outpatient bronchial asthma. A combined clinic was unanimously suggested to remedy this. Conclusion: Proper planning with regard to allocation of support systems and mobilisation of human resources needs to be instituted to realise the implementation of a nationwide combined clinic in the management of paediatric bronchial asthma.
Introduction
Multi-disciplinary healthcare providers need to move beyond task-based responsibility towards a more collaborative approach [1]. In the hospital setting, pharmacists and physicians typically work in tandem with each other [2] and the efficiency of interprofessional collaboration at the ground level will translate into better patient care and management.
Chronic childhood diseases such as bronchial asthma demand effective multidisciplinary team management to improve patient care [3][4]. The medical paediatric team is naturally expected to provide a holistic outpatient management for children with bronchial asthma, including detailed assessment of interval symptoms and revision of the asthma action plan whenever necessary. However, in view of the growing clinical burden and patient load, the quality of medical review and consultation is likely to be adversely affected to some degree [5].
Therefore, the Paediatric Respiratory Medication Therapy Adherence Clinic (PRMTAC) was established under the discretion of Pharmacy Department circa 2015 in Malaysia to complement the management of outpatient paediatric bronchial asthma patients. PRMTAC was primarily chartered to provide support in terms of clinical assessment of inhaler technique, review of medication, chamber care and providing clinical recommendation. Other key assessment points include the assessment of the peak expiratory flow rate for older children, assessment of medication adherence, and confirming the presence or absence of interval symptoms.
Despite the fact that PRMTAC services essentially cover the core clinical assessment in the management of outpatient bronchial asthma, physicians remain as the prescriber and the decision-maker in clinical management. Thorough assessment from PRMTAC in turn provides insight [6] and assists the clinician in making a comprehensive decision with regards to medical care [2]. However, the PRMTAC service was provided separately, and communication with the prescriber was maintained only through a feedback document. Such a work process may open room for inadvertant interprofessional miscommunication.
Therefore, our study aimed to examine the interprofessional collaboration between physicians and pharmacists in the management of paediatric bronchial asthma, to explore the views and experiences of both pharmacists and physicians on the important aspects of PRMTAC and patient-centeredness, and to identify barriers to shared decision-making in the management of paediatric bronchial asthma.
Method
The study involved one-to-one, face-to-face interviews involving the paediatric medical team, and the pharmacists who were directly involved with PRMTAC in Hospital Tuanku Fauziah, Perlis, Malaysia. Individual session (Figure I) was conducted to encourage sharing of personal ideas that may otherwise be deterred in a group interview.
Potential participants were approached by the investigator and the purpose of the study as well as how it would be conducted were explained. Potential participants were given ample time to read through the participant information sheet and ask questions. Upon agreement to participate, a different date, time, and place for a meetup that was convenient for both the investigator and participant was scheduled. The consent form was signed in the presence of the investigator before proceeding with the interview session.
The semi-structured interview was guided by a list of questions relevant to each profession with regards to the management of outpatient paediatric bronchial asthma. Probes included, but were not limited to the performance of standard assessment of bronchial asthma, including the assessment of inhaler technique, peak expiratory flow rate, asthma control and interval symptoms, and medical advice and recommendation. Participants were also encouraged to share personal reflections related to their experiences in managing paediatric bronchial asthma patients. The session was conducted in either English or Malay, according to the participant’s preference. Each session took an average of 45 minutes. A full audio recording was used during the entire session for detailed data retrieval and verbatim transcription.
The session was deemed completed once all the probed questions had reached the thematic conclusion. The transcribed interview answer dialogues were then coded into specific themes and were analysed to reach the research objectives.
Result
Three main themes emerged from the study:- (I) The relevance and necessity of PRMTAC service to complement paediatric outpatient bronchial asthma management, (II) the lack of communication between pharmacist and physician in outpatient bronchial asthma management, and (III) the recommendation for a combined clinic in the management of outpatient paediatric bronchial asthma.
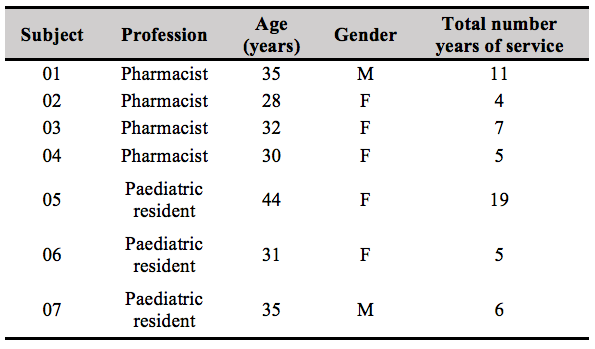
Overall, this study included a total of seven participants, four of which were pharmacists who were actively involved in PRMTAC services, while the remaining three participants were senior paediatric residents who had served at least five years in the clinical department (Table I).
Theme I: The relevance and necessity of PRMTAC service to complement paediatric outpatient bronchial asthma management
PRMTAC service was deemed as necessary for a holistic patient management, with services such as counselling, assessment of prophylactic adherence, asthma control, and assessment of inhaler technique being examples of services offered. Furthermore, it is exclaimed by participants that prior assessments from PRMTAC service saved time for the paediatric team during follow-up assessments without compromising patient care. This is further illustrated in the following responses:
“(PRMTAC service) is quite important. We assess the technique and explore compliance issues. Doctors may not have enough time to monitor and assess the uses and the techniques, overall causing patients to end up not receiving benefits from it..” [sic] (Subject 01, Pharmacist)
“If patient are not using MDIs (Metered Dose Inhaler) with the correct techniques, the disease will not get any better, and the doctor may end up increasing the dose. I’ve experienced handling one patient who was prescribed seven puffs Salbutamol, but the techniques displayed were wrong. In reality, the patient merely needed four puffs.” [sic] (Subject 02, Pharmacist)
“On a normal clinic day, I would see four to five patients per session, I would spend 20 to 30 minutes per patient. Even then, it was still not enough time to assess the patients thoroughly.” [sic] (Subject 06, Paediatric resident)
It is also important to note that pharmacists are deemed better at probing and getting more information than doctors during consultation. Patients are believed to be more open towards pharmacists than doctors, as suggested by the following quotes:
“PRMTAC is necessary. Sometimes, doctors would not have enough time to assess every patient. Sometimes when we assess patients in the clinic, we think that there is compliance issue, symptoms did not improve, so we want a second opinion from a pharmacist to re-assess the situation. Sometimes, patients do not openly discuss their problems with the doctors, but they disclosed them to pharmacists. There were times when pharmacists were able to get more history than doctors.” [sic] (Subject 05, Paediatric resident)
There were also instances the pharmacists noted that the medical team not been teaching the right techniques to the patients. Such incidents were typically encountered during in-ward rounds with the paediatric medical team.
“Sometimes the coordination of breath is wrong. You should empty your lung first. But sometimes, the doctor just ask patient to blow only without realizing patient is inhaling.” [sic] (Subject 01, Pharmacist)
“Most of the time, the housemen will be instructed to teach the MDI technique to the patient. It depends on the medical officer whether he/she will supervise the housemen. Normally, if the housemen were senior enough, and since we trust their capability, we would just freely let them do it. There had been no formal workshops or CMEs. We also learned from seniors, or during times when the in-ward pharmacists were teaching the patients who were newly diagnosed.” [sic] (Subject 07, Paediatric resident)
Theme II: The lack of communication between pharmacist-physician in outpatient bronchial asthma management
Both pharmacists and physicians unanimously agreed that the awareness of the availability of PRMTAC service could be improved:
“There were times when the number of referrals to PRMTAC was very low, affecting our KPI.” [sic] (Subject 04, Pharmacist)
“Only the same medical officers are referring patients to us.” [sic] (Subject 02, Pharmacist)
“I would refer patients to PRMTAC when I suspect that the technique is wrong or compliance is an issue. On average I would refer around 2-3 patients per month. But I don’t think the junior MOs are aware of PRMTAC” [sic] (Subject 06, Paediatric resident)
Pharmacists were also in doubt whether the feedback form returned to their paediatrics counterparts added any value to the paediatrics’ assessment. There had been an absence of direct, physical interactions between pharmacist and paediatric team in the management of patients with bronchial asthma, and everything was done sequentially rather than simultaneously.
“We don’t know whether or not our written feedbacks and suggestion were read or even considered by the Paeds Team.” [sic] (Subject 02, Pharmacist)
Additionally, there was one response from one of the pharmacist respondents in this study regarding an aspect of the paediatric medical team that could be improved upon:-
“Sometimes patients’ diagnoses were written as ‘hypersensitive airway’, I think they may need to be more specific… such as by including other underlying diseases” [sic] (Subject 01, Pharmacist)
Theme 3: Recommendation for a combined clinic in the management of outpatient paediatric bronchial asthma
Both pharmacists and paediatric teams on suggestions for a combined clinic towards a more comprehensive medical care for patients with bronchial asthma. Simultaneous assessment by both professionals will allow a more definitive approach and sharing of ideas between healthcare providers with a more efficient workflow. However, participants of this study pointed out how ensuring the feasibility of a combined clinic would require proper planning, especially in limited-resource facilities.
“I would prefer a combined clinic. But the average number of patients would be more, so there would be a need to assign more dedicated MO (medical officers), and more pharmacists will need to be present also.” [sic] (Subject 01, Pharmacist)
“If the pharmacists can be present during medical consultation, it would be better. We would also like to know about the information that had been counselled and assessed on. I think that the delivery of services would be more efficient that way. As of now, the patient would go there first to see pharmacist, before coming to us. So we can only refer to the pharmacy notes provided.” [sic] (Subject 05, Paediatric resident)
“Since we are seeing patients separately from the Paeds, communication is difficult. The establishment of a combined clinic would ease this, we would be closer to the prescribers to discuss any relevant issues. But pharmacists needed in greater number, and they need to be allocated on specific days for such asthma patients. Now, our PRMTAC is run during the afternoon session, one day per week. It would be better for us to offer such services during the morning session. [sic] (Subject 04, Pharmacist)
“During the pandemic, a virtual counselling session may be considered. There is a recently published guideline from MOH since last January. However, we would still need to address the available resources and find ways to link up with the Paeds team.” [sic] (Subject 03, Pharmacist)
Further recommendations with regards to outpatient assessment of paediatric bronchial asthma patients were suggested:
“I agree that, most of the time, assessments by the Paeds were inadequate due to the sheer patient load at any given clinic session. But, it should be the responsibility of the doctors to at least assess the PEF and techniques during consultation. There should be a formal guideline, specifying ‘this is what you should do in clinic’, or ‘this is what should be written in report’. We can probably come up with a specific guideline, like a checklist to be used in the clinic, something simple to optimise the time efficiency.” [sic] (Subject 05, Paediatric resident)“PRMTAC review follow-up should be more stringent. We kept losing patients. There had also been no guidelines on which areas to comment or emphasize on when counselling. There had also been no credentialing and privileging program for PRMTAC officers.” [sic] (Subject 02, Pharmacist)
Discussion
PRMTAC services were rated as highly relevant in the management of outpatient bronchial asthma among all study respondents, irrespective of profession. The detailed assessment of medication compliance, which may be affected by complex regimens or inadequate instructions [2,3] and the technical demonstration provided by PRMTAC services were deemed fundamental in holistic patient care [7], particularly in cases of poorly controlled and partially controlled asthma.
PRMTAC session typically oversees fewer patients as compared to the medical follow-up, hence were able to engage better with patients and establish better communication and rapport, which is fundamental in patient care [8]. PRMTAC service acts as an extra safety check in the system [7][9] as it also assesses inhaler technique and medication compliance, improves disease control, identifies triggering factors, and assesses peak expiratory flow rates in older children.
Pharmacists in-charge of PRMTAC service should be credentialed and accredited. Certain sets of requirements and workshops need to be instituted to credential them as part of the PRMTAC team as it requires skills to perform PRMTAC services [10]. PRMTAC service should be considered as a specialized form of MTAC. The first reason is that the process of dealing with paediatric patients requires certain soft skills to enable mutual interaction. Secondly, besides assessing medication adherence and disease control through interval system scores and peak expiratory flow rates, pharmacists should also be well-versed with the use of different types of inhalers and choice of medications, as well as the proper technique and care of different chamber brands. Indeed, it has been suggested based on the literature that such specialized skills need to be acquired by pharmacists delivering PRMTAC services [3].
The current clinical scenario demonstrates that the pharmacist and paediatric medical team works independently and in parallel [2], rather than collaboratively. Such workflow challenges shared decision-making with regards to patient-focused medication. The lack of physical interaction between pharmacist and physician also impedes sharing of ideas and new knowledge [2][6] that could benefit both parties in relation to the current and updated management of outpatient bronchial asthma. A combined clinic was unanimously suggested to remedy this. A combined clinic would suggest the simultaneous presence of multiple subspecialties or related professions providing informed and comprehensive medical decisions regarding patient care [1][4]. Indeed, a combined clinic is routine in the medical setting in patients with complex medical illness requiring multiple views from each managing team. Therefore, in the setting of the outpatient management of paediatric bronchial asthma, the establishment of a combined clinic may resolve certain issues related to interprofessional miscommunication, an issue that was highlighted in our study. However, allocation of resources whilst considering feasibility, manpower, and logistics, should be carefully considered to minimize inefficiency and instances of poor execution.
Conclusion
Proper planning regarding allocation of support system and mobilisation of human resources needs to be instituted to realise the implementation of a nationwide combined clinic in the management of paediatric bronchial asthma.
Regular continuous medical education (CME) sessions are recommended for healthcare workers involved in the management of outpatient bronchial asthma to inform them of current updates with regards to any breakthroughs in clinical management.
Acknowledgement
The authors would like to thank the Director General of Health Malaysia for his permission to publish the paper. We are also grateful to Puan Nik Mah binti Nik Mat, Head of Pharmacy Department and Dr Siti Akma binti Ishak, Head of Paediatrics Department of Hospital Tuanku Fauziah, Perlis for their overwhelming support throughout this research project.
Conflict of Interest
This study has no conflict of interest. This research did not receive any specific grant from funding agencies in public, commercial or not-for-profit sectors.
Reference
- Hoffmann TC, Montori VM, Del Mar C. The connection between evidence-based medicine and shared decision making [Internet]. Vol. 312, JAMA – Journal of the American Medical Association. American Medical Association; 2014 [cited 2021 May 31]. p. 1295–6. Available from: https://doi.org/10.1001/jama.2014.10186
- Mercer K, Burns C, Guirguis L, Chin J, Dogba MJ, Dolovich L, et al. Physician and pharmacist medication decision-making in the time of electronic health records: Mixed-methods study. J Med Internet Res [Internet]. 2018 Sep 1 [cited 2021 May 31];20(9):e9891. Available from: https://doi.org/10.2196/humanfactors.9891
- Kaplan A, Price D. Treatment adherence in adolescents with asthma [Internet]. Vol. 13, Journal of Asthma and Allergy. Dove Medical Press Ltd.; 2020 [cited 2021 May 31]. p. 39–49. Available from: https://doi.org/10.2147/jaa.s233268
- Gums TH, Carter BL, Milavetz G, Buys L, Rosenkrans K, Uribe L, et al. Physician-pharmacist collaborative management of asthma in primary care. Pharmacotherapy [Internet]. 2014 Oct 1 [cited 2021 May 31];34(10):1033–42. Available from: https://doi.org/10.1002/phar.1468
- Stevenson FA, Barry CA, Britten N, Barber N, Bradley CP. Doctor patient communication about drugs: The evidence for shared decision making. Soc Sci Med. 2000 Mar 1;50(6):829–40. Available from: https://doi.org/10.1016/s0277-9536(99)00376-7
- Crespo-Gonzalez C, Fernandez-Llimos F, Rotta I, Correr CJ, Benrimoj SI, Garcia-Cardenas V. Characterization of pharmacists’ interventions in asthma management: a systematic review. Journal of the American Pharmacists Association 2018 Mar 1;58(2):210-9. Available from: https://doi.org/10.1016/j.japh.2017.12.009
- Hasan S, Stewart K, Chapman CB, Kong DCM. Physicians’ perspectives of pharmacist-physician collaboration in the United Arab Emirates: Findings from an exploratory study. J Interprof Care [Internet]. 2018 Sep 3 [cited 2021 May 31];32(5):566–74. Available from: https://doi.org/10.1080/13561820.2018.1452726
- Ng YK, Shah NM, Loong LS, Pee LT, Chong WW. Patient-centred care in the context of pharmacy consultations: A qualitative study with patients and pharmacists in Malaysia. J Eval Clin Pract [Internet]. 2020 Dec 1 [cited 2021 May 31];26(6):1638–47. Available from: https://doi.org/10.1111/jep.13346
- Mehuys E, Van Bortel L, De Bolle L, Van Tongelen I, Annemans L, Remon JP, et al. Effectiveness of pharmacist intervention for asthma control improvement. Eur Respir J [Internet]. 2008 Apr 1 [cited 2021 May 31];31(4):790–9. Available from: https://doi.org/10.1183/09031936.00112007
- Elaro A, Bosnic-Anticevich S, Kraus K, Farris KB, Shah S, Armour C, et al. Pharmacists’ perspectives of the current status of pediatric asthma management in the U.S. community pharmacy setting. Int J Clin Pharm [Internet]. 2017 Aug 1 [cited 2021 May 31];39(4):935–44. Available from: https://doi.org/10.1007/s11096-017-0471-1
Please cite this article as:
Karniza Khalid, Nurul Azima Mazlan, Wan Nor Amalina Zainun, Amalina Anuar, Nuqman Mursyid Ramli and Wei Chern Ang, Qualitative Analysis on Interprofessional Collaboration in the Management of Paediatric Bronchial Asthma: Challenges and Suggestions for Improvement. Malaysian Journal of Pharmacy (MJP). 2022;1(8):7-12. https://mjpharm.org/qualitative-analysis-on-interprofessional-collaboration-in-the-management-of-paediatric-bronchial-asthma-challenges-and-suggestions-for-improvement/