Abstract
Objectives: The objectives of this study were to determine the cost of a behavioral risk factor reduction program at the worksite and to compare the cost-effectiveness of the program with a control group. Methodology: This was a quasi-experimental study conducted among employees of Universiti Sains Malaysia. The program targeted five primary risk factors (RF). Participants in the intervention program were subjected to schedule individualized counseling and seminars during the 6- month follow-up. Participants in the control group underwent health screening. Cost-effectiveness analysis was conducted from the payer’s perspective to determine the cost of 1% increase in proportion of participants who reach ideal targets for the RF. One-way sensitivity analysis was also conducted. Results: A total 136 participants were recruited in this study. At 6-month follow-up, significantly higher proportion of participants in the intervention group reached target for fruit and vegetable intake (P < 0.001) and physical activity (P = 0.017). The costs of the intervention program and control group were estimated to be MYR304.52 (USD92.28) and MYR169.90 (USD51.48) per participant respectively. The incremental cost-effectiveness ratio (ICER) of all the RF were lower than the World Health Organization recommendation based on the CHOICE analyses for relative cost-effectiveness of an intervention. Body mass index and alcohol consumption reported negative ICER which indicated control dominant. Sensitivity analyses showed that ICER was reported to be most sensitive to the change in participants’ salary. Conclusion: The proposed health promotion program was shown to be cost-effective in modifying most of the behavioral RF.
Background
Over the years, the life expectancy of the Malaysian population has increased and coupled with the adoption of western lifestyle, the prevalence of cardiovascular risk factors has also increased[1][2]. This increased resulted in an increased in the prevalence of cardiovascular (CV) and its related diseases[3]. Cardiovascular and its related diseases required long-term medical treatment.
Modification of risk factors (RFs) is crucial in order to curb the rise of CV disease. In Malaysia, numerous CV prevention program has been initiated by various parties. These included the individualized and community-wide strategies. Community-wide strategies are widely used but its effectiveness is questionable. Individualized counseling on RF modification provides personalized information to individuals and is believed to produce better outcome. However, the implementation in real world scenario of such a program is questionable because individualized health promotion program is time, manpower and resources consuming.
This health promotion program incorporated both behavioral and educational aspects of lifestyle modification strategies, with an emphasis on the five modifiable RF. The aim of the health promotion program was to correct an array of cardiovascular risk factor behaviors simultaneously. The emphasis of this program was empowerment, which aimed to help participants to develop the knowledge, skills, attitude and self-awareness required to take up the responsibility for their own health. The intervention program included stage-matched motivational and behavioral strategies based on the Transtheoretical Model (TTM). These were applied to the five modifiable RFs, namely smoking, unhealthy diet, excessive alcohol consumption, physical inactivity, and obesity and being overweight. It was assumed that changes to a primary RF will bring positive changes to the secondary RF.
In Malaysia, public healthcare sector was heavily subsidized by the government. The rise in CV and its related diseases has dramatic impact on healthcare expenses as well as employees’ absenteeism from work. With the limited resources for healthcare, priority setting is important to identify the treatment (intervention) which gives maximum health gain within a limited budget. Thus evaluation of cost and benefit of a health promotion program can support decision-makers in effective budget deployment. Moreover, the cost-effectiveness analysis of the health promotion program provided an insight on the affordability of this program.
The objective of this study was to compare the cost-effectiveness of a behavioral RF reduction program at the worksite versus health screening alone in achieving the ideal target for five primary cardiovascular risk factors.
Methodology
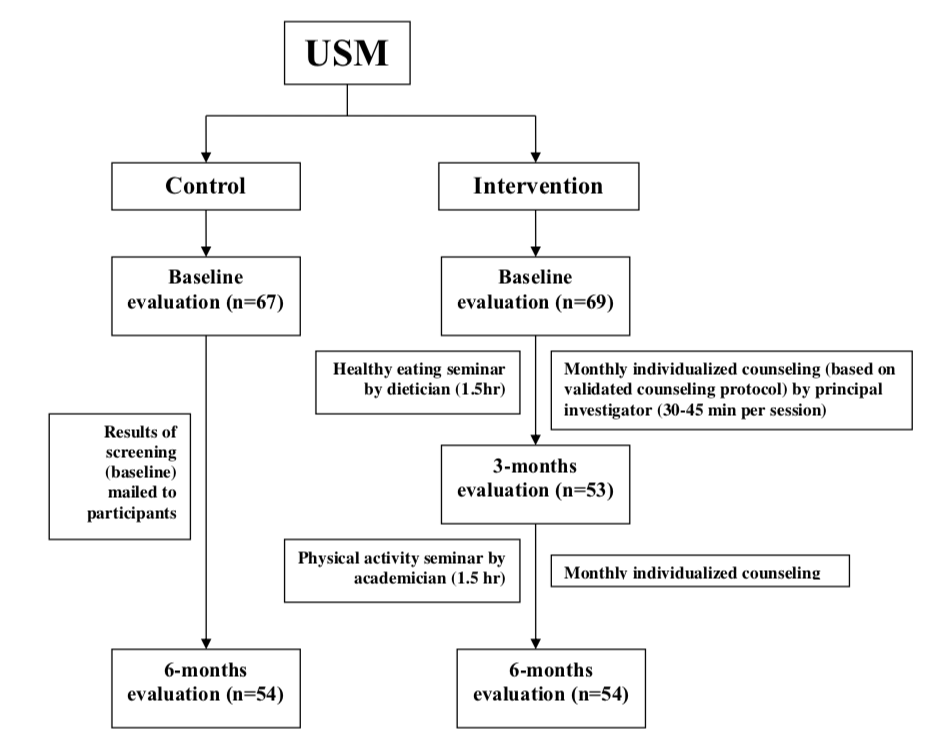
This was a quasi-experimental study carried out from October 2009 to July 2010 at Universiti Sains Malaysia (USM). Participants for the intervention and control group were recruited among the employees of Engineering Campus and main campus of USM respectively.
This prospective lifestyle interventional study targeted five primary RF namely smoking, excessive alcohol consumption, physical inactivity, inadequate fruit and vegetable intake and overweight/obesity. Participants in the intervention group were required to attend scheduled individualized counseling and seminars during the 6-month follow-up. Individualized counseling was based on a standardized and validated (using Delphi method) counseling protocol. The frequencies of the individualized counseling sessions were bimonthly for the first month and monthly thereafter. Two seminars were held during the 6-month program targeted on the two main RF i.e. physical inactivity and unhealthy diet. The health educator was trained on providing counseling on RF management based on the TTM and motivational interviewing principles. Control group participants underwent health screening and the results of this health screening were mailed to them within one week. No involuntary changes were made to their lifestyle. Figure 1 display the flow of the study.
Participants for both the intervention and control group fulfilled pre-set inclusion and exclusion criteria prior to enrollment into the study. The inclusion criteria were no previous CV disease/events and not currently on medication for treatment of hypertension, diabetes or dyslipidemia. Participants should have at least one cardiovascular risk factor. Employees who were pregnant, history of severe renal or liver disease and who were currently enrolled in any other lifestyle changes program were excluded from this study.
Data on current RF status were collected using the WHO STEPS instrument for chronic disease risk factors surveillance questionnaires[4]. Behavioral RF status was self-reported. The same instruments and measurements were used throughout the study to reduce variability between the instruments and measurements made for the various obesity indexes. Physical measurements made included height, weight and waist circumference (WC). Height and weight were measured using a stadiometer. Waist circumference was measured using a fiberglass measuring tape taken between the inferior margin of the last rib and the crest of the ilium in a horizontal plane. Hip circumference measurement was taken around the pelvis at the point of maximal protrusion of the buttocks while patient stand with feet 25 cm to 30 cm apart with weight evenly distributed[5].
Cost-effectiveness analysis was conducted from the perspective of the university, as payer of healthcare for its employees. Both direct and absenteeism costs were included in the costing analysis. Research-related costs were excluded from the analysis. These included cost for awareness program and incentives paid to the participants. Costs of hospital admission and medications were also excluded in the analysis because analysis was done until the day the participants were admitted for any CV events or started on medications. Micro-costing was carried out wherever possible. In cases where micro-costing cannot be done, expert opinion of panel or the closet estimates were used[6].
Resource consumed in health and productivity sector were accounted in the cost as follows (Table 1). The costs of the building (or space) and equipment used during the intervention were annuitized over the useful life of the building (or space) and equipment which was estimated to be between 5 and 20 years at a 5% discount rate. It was assumed that there was no resale value for the equipment after the useful life of the equipment. The estimated ‘equivalent annual cost’ (EAC) was derived by taking into account the depreciation aspect and the opportunity cost aspect of the capital cost. The costs and outcomes of the intervention program were not discounted because only 6-month outcomes were taken into consideration during analysis.
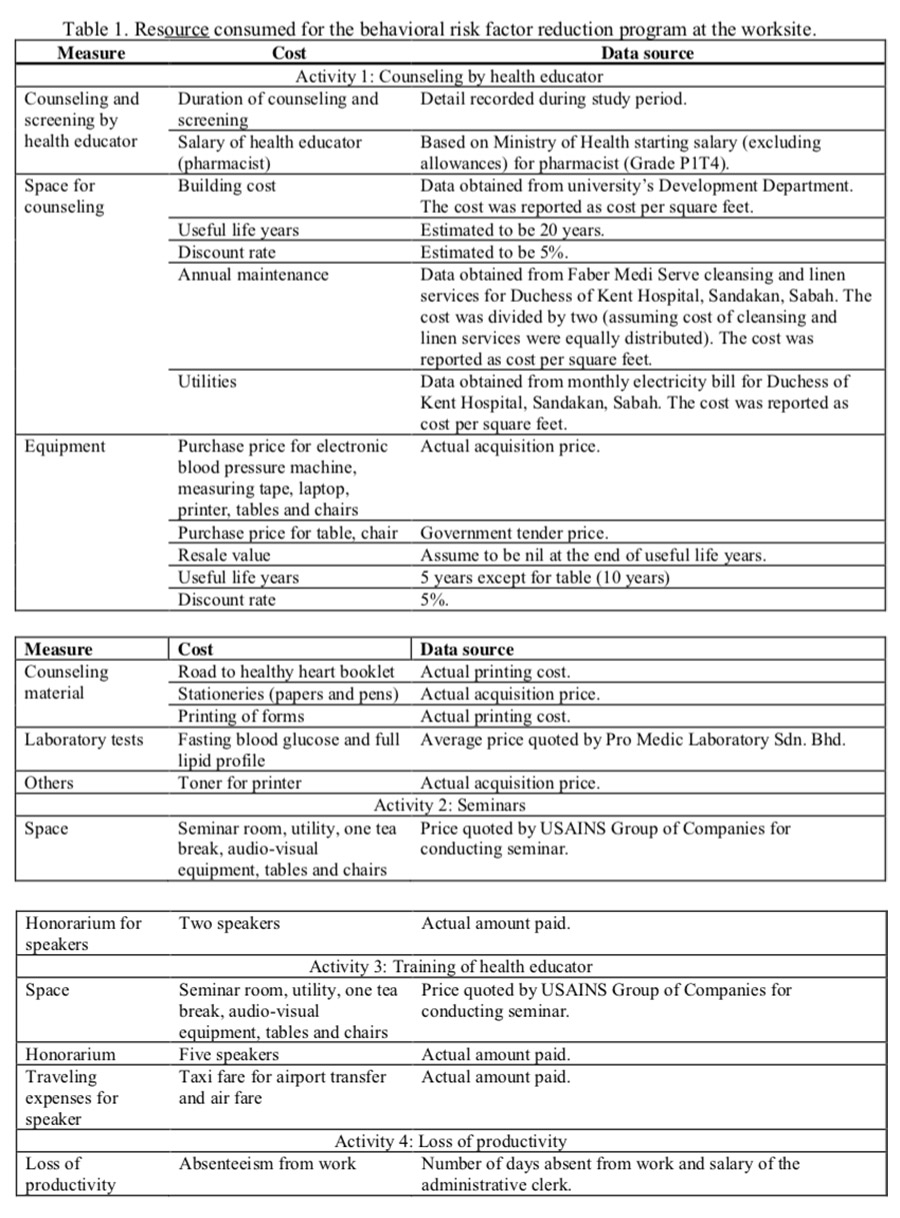
The costs of the intervention and control group were summed based on the following equation.
Average variable cost
= ∑ cost of program per participanti / number of participants
= (∑ cost of counselingi / number of participants) + counseling material + [∑ (laboratory charges x number of testi) / number of participants)] + [∑ (participant daily salary x days of medical sick leavei) / number of participants)]
= [∑ (cost of health educator per minute + cost of space per minute + cost of maintenance per minute + cost of electricity per minute + cost of equipment per minute) x duration of counselingi/ number of participants] + counseling material + [∑ (laboratory charges x number of testi) / number of participants)] + [∑ (participant daily salary x days of medical sick leavei) / number of participants)]
Average fixed cost
= ∑ (cost for stationeries + printing charges + seminars + training) / number of participants
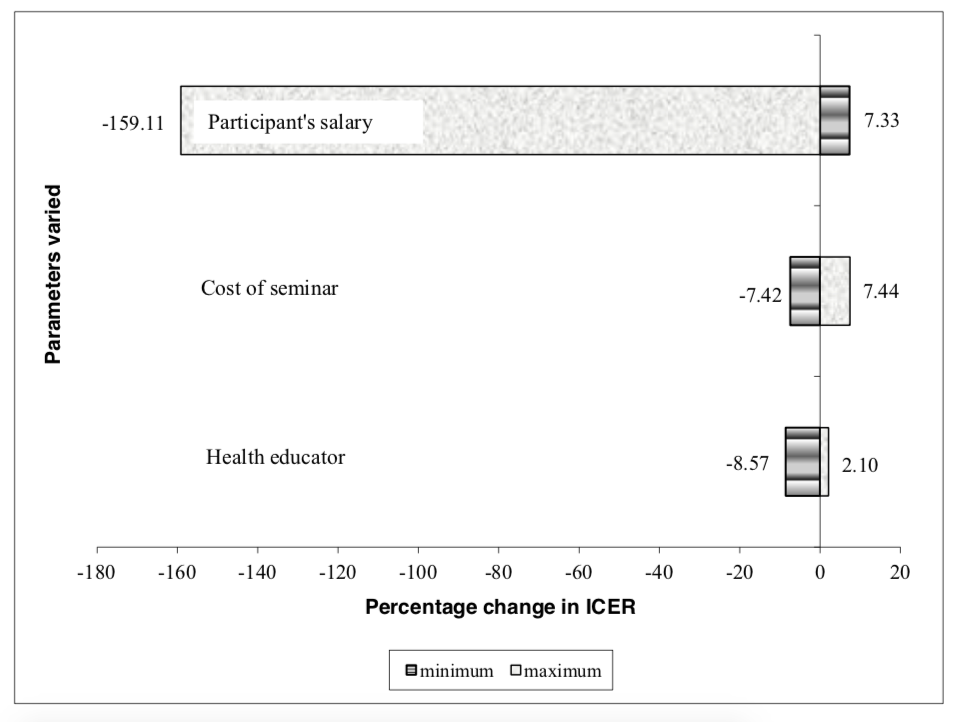
One-way sensitivity analysis was conducted by varying the cost of three parameters to test the robustness of the results obtained. These parameters were the salary of health educators, the salary of the participants and cost of renting of seminar room. These parameters were chosen due to the estimated costs used in the initial evaluation. In this study, the intervention was conducted by a pharmacist. However, other healthcare professionals who frequently conduct such programs are medical officers, dieticians or nurses. Therefore, the health educator’s salary was varied between the highest and the lowest salary of these professions, based on the starting salary as quoted by the Public Service Department, Malaysia. Secondly, the cost of the medical sick leave of the base case analysis was calculated based on the salary of an administrative clerk, which was the occupation of the majority of the participants. However, there were participants of other occupation groups in this program. Therefore, the highest and the lowest salary of these professions were used in the sensitivity analysis. Finally, the cost of the seminar room and tea break can vary depending on the place occupied and the food ordered.
The primary outcome measure was to examine the intervention effects in terms of the prevalence of individuals meeting healthy lifestyle recommendations after intervention. Given that there are four primary outcome measures, a range of sample-size estimates based on the intervention effects obtained from previous studies was calculated. The required sample size was calculated using the ormula for finding the sample size for studies about proportions in two groups assuming a Type I error of 0.05 and a power of 80%[7].
It was assumed that the achievement of fruit and vegetable intake in the intervention group was 33.0% as compared with 13.0% in the control group; physical activity was 90.0% in the intervention group as compared with 71.0% in the control group[7]; smoking cessation rates were 17.0% for the intervention group as compared with 2.3% in the control group[8] and a higher compliance with recommendations for the control group (30.0% vs 26.0%) was reported for alcohol consumption[7]. After taking into considerations a 20% drop-out rate, the required sample size was between 58 and 118 in each group.
Pre-determined criterion to define whether a change has successfully reach its target or not, were based on the targets adopted from the Malaysian clinical practice guidelines[5] [9][10][11][12][13][14]. The outcome measure for this study was the cost per 1% increase in proportion of participants who reach the ideal targets for the RF. Approval from the Joint Ethics Committee of the School of Pharmaceutical Sciences, USM-Lam Wah Ee Hospital was obtained prior to the commencement of the study.
All data were analyzed using statistical software SPSS package version-16. A two-tailed P-value < 0.05 was considered statistically significant. Baseline sociodemographic and RF characteristics between intervention and control groups were reported using simple descriptive statistics. Continuous variables were expressed in mean and standard deviation or median and inter-quartile range for continuous variables. Discrete variables were expressed in proportion. Differences in the proportion of participants reaching target for each RF were compared using chi square test (or Fisher exact test).
Results
A total 136 participants were recruited into the study with 69 participants (50.7%) in the intervention group and 67 participants (49.3%) in the control group. At 6-month follow-up, 78.3% (n = 54) and 91.1% (n = 61) of the participants completed final evaluation. Majority of the participants were female and of Malay ethnic origin. The mean age was 36.92 (SD = 9.14) years. There was no significant difference between intervention and control group in terms of sex and ethnicity.
The RFs were categorized into reaching target and not reaching target and were compared between intervention and control groups (Table 2). At baseline, there was no significant difference in the proportion of participants reaching the target for any of the RF. However, at 6-month follow-up, significantly higher proportion of participants in the intervention group reached the target for fruit and vegetable intake (P < 0.001) and physical activity (P = 0.017).
A total of 69 participants in the intervention group were entered into the analyses. The cost of the intervention program was estimated to be MYR304.52 (USD92.28) per participant.

Similar estimation and calculation was used to calculate the cost of the control group. The time spent on screening for baseline and 6-month evaluation was taken into consideration of cost calculation. Since no active intervention was provided to the control group, laptop and printer were considered not utilized by this group of participant. They were also not provided with the counseling material and therefore its cost was excluded from this analysis for the control group. It was estimated that the screening of the control group used up one ream of A4 paper and one pen with a total cost of MYR18.50. The printing cost over the 6-month was MYR356.00 (108 pages for 66 participants at MYR0.05 per page). The cost of seminars and training of health educator was also excluded from this analysis. Initially there were 67 participants in the control group. However, three of the participants were transferred to another institution and data on their medical sick leave and 6-month evaluation were not available. Therefore, they were excluded from these analyses giving a total of 64 participants in the control group. The cost of screening for the control group was estimated to be MYR169.90 (USD51.48) per participant. Therefore, the differences in cost between intervention and control group participant was MYR134.62 (USD40.79) per participant.
Cost-effectiveness Analysis of Proportion of Participants Reaching Risk Factors Target The summary of the cost-effectiveness ratio (CER) and incremental cost-effectiveness ratio (ICER) for the proportion of participants reaching target for each RF was presented in Table 3. Cost- effectiveness ratio provides information on the cost of 1% increase in the proportion of participants reaching target for each RF. It can be seen that within the intervention group, alcohol consumption worsen with a negative CER. Similarly, three RFs (fruit and vegetable intake, physical activity and WC) produced negative CER for the control group.
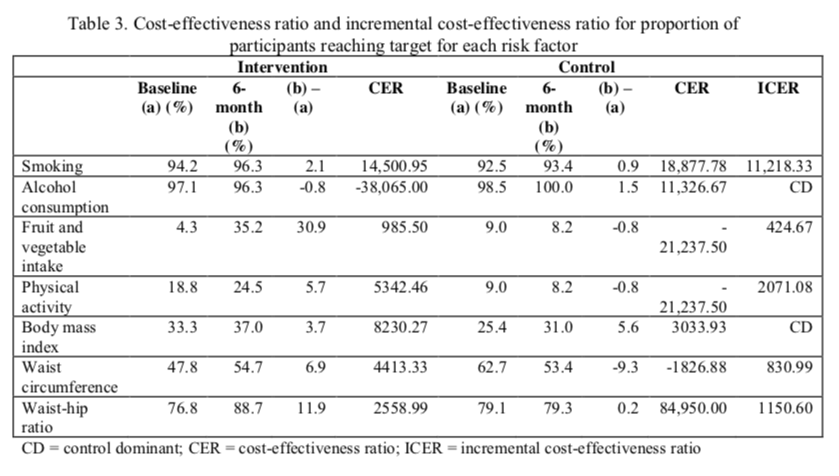
Incremental cost-effectiveness ratio is defined as the ratio of change in cost of an intervention as compared to the control group to the change in outcomes between the two groups[15]. A negative ratio indicated that the control group was dominant in increasing the proportion of participants reaching target. This was seen with body mass index (BMI) and alcohol consumption.
Sensitivity analyses were conducted to test the robustness of the cost-effectiveness model. Three parameters were varied between their maximum and minimum values. These were the salary of the health educator, salary of participants for productivity cost estimation and cost of conducting seminars.
The cost per participant for the intervention and control groups was recalculated based on the variation of the pre-set parameters in the sensitivity analysis. The incremental costs vary from – MYR79.57 (USD24.11) (cost per participant in the control group higher than intervention group) to MYR144.49 (USD43.78). This was summarized in Table 4.
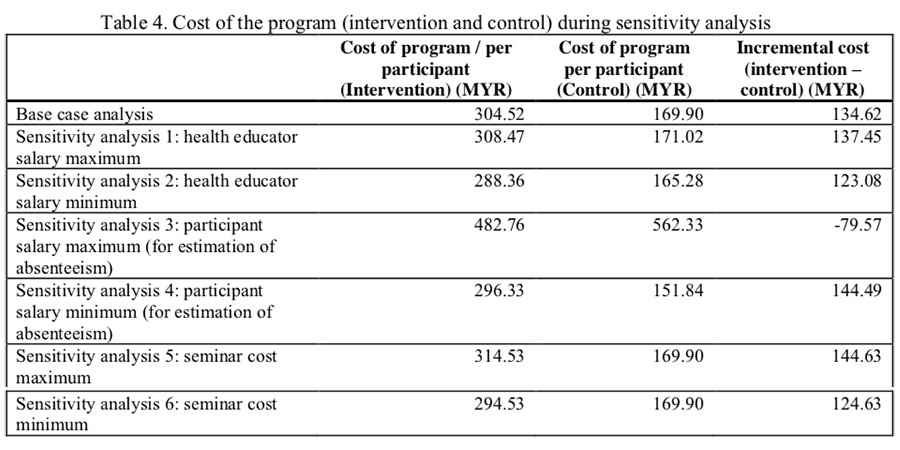
Cost-effectiveness ratio and ICER were calculated for each RF and for each of the parameters which was included in the sensitivity analysis. Subsequently, the percentage change from the base case analysis in the ICER was calculated.
The sensitivity of the change in parameters varied. Although the cost of the health educator made up of 18% of the total cost of the program, varying this cost to the medical officer’s salary did not affect the results as much as varying it to the salary of the staff nurse. Hence employing staff nurse to conduct the intervention is more cost-effective. Secondly, varying the cost of the rental for the seminar room did not have much effect on the ICER. In contrast, varying the participants’ salary between the minimum (salary of general worker) and maximum (lecturer) have tremendous effect on the ICER. This salary was used to calculate the cost of medical sick leave taken by the participants. There was more than 150% change when the participants’ salary was adjusted to the maximum, in favor of the intervention group. When the salary was adjusted to the minimum, the cost difference increased from base case analysis resulting in an increased in percentage change in ICER. This can be observed from the tornado diagram as presented in Figure 2.
Similarly, ICER was recalculated by varying the two main outcomes, namely physical activity and adequate fruit and vegetable intake. It was found that by varying proportion of participants achieving target RF, the ICER achieved was still less than MYR30,000.
Discussion
The aim of this study was to conduct cost-effectiveness analysis on the effect of a worksite health promotion program on achieving RF targets. Significant improvement of the intervention on the proportion of participants reaching the targets was found in fruit and vegetable intake and physical activity. Most of the studies reviewed reported significant higher proportion of participants in the intervention groups meeting the target for physical activity and fruit and vegetable intake except for studies reported by Jimmy et al. (2005) (physical activity) and Hardcastle et al. (2008) (fruit and vegetable intake)[7] [16][17][18][19].
The effect of health promotion program on the prevalence of smoking was not consistent. Our study reported no significant difference between the two groups. This was supported by studies reported elsewhere[18][20][21][22][23][24]. However, the numbers of smokers might be too small to detect any differences during analyses.
The intervention program was more costly than the control, with a differential cost of MYR134.62 (USD40.79) per participant in six months. The differential costs between health promotion program and screening along differed widely in existing studies, depending on the duration, intensity and type of intervention. It ranged from USD41.09 to EUR430 (USD612.42)[25][26][27].
It is not feasible to compare the CER and ICER calculated from this study to the studies reported elsewhere. Most of the studies had modeled the effect of the intervention to final outcomes such as life-years gained and quality-adjusted life years.
The ICER of the various obesity indexes produced different results. The disproportionate achievement of target RF between BMI, WC and waist-hip ratio (WHR) between intervention and control group was unexpected and was not supported by the studies reviewed. A reduction in body weight is frequently reported to correspond with reduction in abdominal obesity (reported as WC and WHR)[28][29][30]. The only exception was a study by Hassan et al. (2011) which reported a significant reduction in WC and hip circumference but not BMI after a 6-month program targeted on diet and individualized physical activity[31].
Despite the negative ICER for alcohol consumption, the number of participants who achieved targets for alcohol consumption was too small to make any general conclusion on the effect of the program.
The other RF consistently showed positive ICER for both the outcomes. The calculated ICER were much lower than the World Health Organization recommendation based on the CHOICE analyses for relative cost-effectiveness of an intervention, whereby an ICER of less than MYR30,000 (USD9090.91) is considered cost-effectiveness for public policy intervention in Malaysia[32].
A review of the literature found numerous economic evaluation which reported positive results from the intervention (including worksite intervention). Smoking cessation program which utilized remuneration or nicotine-replacement therapy was more cost-effective than usual counseling alone[33]. Sevick et al. (2000) reported the cost-effectiveness of lifestyle intervention as compared with structured program in terms of physical activity, BP and weight[34]. In 2007, Sevick et al (2007) reported that it was more cost effective to use printed letters than phone to improve physical activity level[35]. However, other studies also reported no superiority of intervention on the economic outcomes on the RFs[27][28][29][30][31][32][33][34][35][36]. Almost all of the economic evaluation of worksite intervention program reported in reduction in absenteeism[27][37][38].
The sensitivity analyses showed that the ICER was most resistant to change in the cost of seminar (both minimizing and maximizing the cost) and also maximizing the salary of the health educator. In contrast, the ICER was most sensitive to the participant’s salary, whereby the maximum possible salary resulted in approximately 150% change in ICER as compared to the base case model. These results showed that it is possible to further improve the incremental cost of CER by utilizing a staff nurse trained in conducting this program. Training should be emphasizing in order to ensure standardization of counseling given. More importantly, the sensitivity analyses results also showed that salary of the participants greatly impact the ICER. The participants’ salary in the base model was based on the salary of an administrative clerk. This salary was used to calculate the cost of medical sick leave. This can be explained by the fact that the number of medical sick leave days taken by the participants in the intervention group (n = 1.03 days) was lower than the control group (n = 2.27 days) even though this difference did not reach statistical significance (Mann-Whitney test, P = 0.175). A public university consisted of several positions with different salary scheme. If this program is conducted in a large scale, involving large number of participants, it is expected to be more cost-effective.
The results from this analysis have to be taken with some caution. This study looked into the intermediate outcomes related to the individual RF. Despite not addressing the mortality and morbidity over lifetime, these intermediate outcomes (behavioral changes) were deemed clinically relevant. Numerous studies have reported the correlation between these intermediate outcomes and mortality and morbidity[15]. Furthermore, the behavioral RF status was self-reported and is subjected to recall bias. Moreover, participation in the program is voluntary and non-random. Therefore, it was expected participants with higher intention to change was enrolled in the program.
Conclusions
In conclusion, this program was shown to be cost-effective in modifying most of the behavioral RF, most notable physical activity and fruit and vegetable intake. Cost-effectiveness of the program would be increased with recruitment of high-risk individuals with higher baseline risk. Secondly, by recruiting a higher number of participants into the program, the cost of the intervention can be reduced. As such it is recommended that this program be extended throughout the worksite particularly targeted at high-risk individuals.
Conflict of Interest
The authors declared no conflict of interest in conducting and writing this research.
Acknowledgement
I would like to thank the staff from the Health Unit of Engineering Campus, USM for their continuous support during the course of this study. This research was financially supported by Universiti Sains Malaysia Research University [1001/PFARMASI/813018]; and Healthy Campus Grant 2008.
References
- Ministry of Health. MyNCDS-1 report. Putrajaya: Ministry of Health, Malaysia; 2007 [cited 2008 30 January ]; Available from: www.dph.gov.my/ncd/surveillance/index.
- Institute for Public Health. The Third National Health and Morbidity Survey 2006 (NHMS III): executive summary. Putrajaya: Institute for Public Health, National Institutes of Health, Ministry of Health2008.
- Ministry of Health. Statistik – Fakta Kesihatan. Putrajaya: Ministry of Health; 2010 [updated 12 March 2010; cited 2010 25 November ]; Available from: http://www.moh.gov.my/v/stats_si.
- World Health Organization. STEPwise Approach to Surveillance (STEPS). Geneva: World Health Organization; 2008 [cited 2008 30 January ]; Available from: www.who.int/chp/steps/en/.
- Ismail IS, Bebakar WMW, Kamaruddin NA, et al. Clinical practice guidelines on management of obesity 2004. Putrajaya: Ministry of Health Malaysia, Academy of Medicine of Malaysia, Malaysian Association for the Study of Obesity, Malaysian Endocrine and Metabolic Society; 2004.
- Heerey A, McGowan B, Ryan M, et al. Microcosting vs DRGs in the provision of cost estimates for use in pharmacoeconomic evaluation. Expert Rev Pharmacoecon Outcomes Res. 2002;2:29- 33.
- Kypri K, McAnally HM. Randomized controlled trial of a web-based primary care intervention for multiple health risk behaviors. Prev Med. 2005;41:761-6.
- Ranney L, Melvin C, Lux L, et al. Systematic review: smoking cessation intervention strategies for adults and adults in special populations. Ann Intern Med. 2006;145:845-56.
- Krauss RM, Eckel RH, Howard B, et al. AHA dietary guidelines: revision 2000: a statement for healthcare professionals from the Nutrition Committee of the American Heart Association. Circulation. 2000;102:2284-99.
- Grundy SM, Becker D, Clark LT, et al. Third report of the National Cholesterol Education Program (NCEP) expert panel on detection, evaluation and treatment of high blood cholesterol in adults (Adult Treatment Panel III) panel report. Circulation. 2002;106:3143-421.
- Mahayiddin HA, Mazlan M, Bakar SA, et al. Clinical practice guidelines on treatment of tobacco use and dependence 2003. Putrajaya: Ministry of Health Malaysia; 2003.
- Chan SP, Zain AZM, Ismail IS, et al. Clinical practice guidelines in the management of type 2 diabetes mellitus. Third ed. Sivalal S, Jaudin R, editors. Putrajaya: Ministry of Health Malaysia, Persatuan Diabetes Malaysia, Academy of Medicine; 2004.
- Chobanian AV, Bakris GL, Black HR, et al. Seventh report of the Joint National Committee on prevention, detection, evaluation, and treatment of high blood pressure. Hypertension. 2003;42:1206-52.
- Zambahari R, Jeyamalar R, Rahman ARBA, et al. Clinical practice guidelines on management of dyslipidemia. Putrajaya: Ministry of Health Malaysia, Academy of Medicine Malaysia, National Heart Association of Malaysia; 2004.
- Wagner T, Goldstein MK. Behavioral interventions and cost-effectiveness analysis. Prev Med. 2004;39:1208-14.
- Oldroyd JC, Unwin NC, White M, et al. Randomised controlled trial evaluating the effectiveness of behavioural interventions to modify cardiovascular risk factors in men and women with impaired glucose tolerance: outcomes at 6 months. Diabetes Res Clin Pract. 2001;52:29-43.
- Jimmy G, Martin BW. Implementation and effectiveness of a primary care based physical activity counseling scheme. Patient Educ Couns. 2005;56:323-31.
- Wood DA, Kotseva K, Connolly S, et al. Nurse-coordinated multidisciplinary, family-based cardiovascular disease prevention programme (EUROACTION) for patients with coronary heart disease and asymptomatic individuals at high risk of cardiovascular disease: a paired, cluster- randomised controlled trial. Lancet. 2008;371:1999-2012.
- Hardcastle S, Taylor A, Bailey M, et al. A randomised controlled trial on the effectiveness of a primary health care-based counselling intervention on physical activity, diet and CHD risk factors. Patient Educ Couns. 2008;70:31-9.
- Kreuter MW, Strecher VJ. Do tailored behavior change messages enhance the effectiveness of health risk appraisal? Results from a randomized trial Health Educ Res. 1996;11:97-105.
- Glasgow RE, Terborg JR, Strycker LA, et al. Take Heart II: Replication of a worksite health promotion trial. J Behav Med. 1997;20:143-61.
- Sorensen G, Stoddard A, Hunt MK, et al. The effects of a health promotion-health protection intervention on behavior change: The WellWorks Study. Am J Public Health. 1998 November 1, 1998;88(11):1685-90.
- Emmons K, Linnan LA, Shadel WG, et al. The Working Health Project: A worksite health- promotion trial targeting physical activity, diet and smoking. J Occup Environ Med. 1999;41:545-55.
- Harting J, Assema Pv, Limpt Pv, et al. Cardiovascular prevention in the Hartslag-Limburg project: effects of a high-risk approach on behavioral risk factors in a general practice population. Prev Med. 2006;43:372-8.
- FooteA,ErfurtJC.Thebenefitofcostratioofwork-sitebloodpressurecontrolprograms.JAm Med Assoc. 1991;265:1283-6.
- Pritchard DA, Hyndman J, Taba F. Nutritional counselling in general practice: a cost- effectiveness analysis. J Epidemiol Community Health. 1999;53:311-6.
- Proper KI, Bruyne MCd, Hildebrandt VH, et al. Costs, benefit and effectiveness of worksite physical activity counseling from the employer’s perspective. Scand J Work Environ Health 2004;30(1):36-46.
- Leutholtz BC, Keyser RE, Heusner WW, et al. Exercise training and severe caloric restriction: Effect on lean body mass in the obese. Arch Phys Med Rehab. 1995;76(1):65-70.
- Slentz CA, Duscha BD, Johnson JL, et al. Effects of the amount of exercise on body weight, body composition, and measures of central obesity: STRRIDE- A randomized controlled study. Arch Intern Med. 2004 January 12, 2004;164(1):31-9.
- Jakicic JM. The effect of physical activity on body weight. Obesity. 2009;17(n3s):S34-S8.
- Hassan NE-M, Zak ST, El-Masry S, et al. Impact of balanced caloric diet and physical activity on body composition and fat distribution of obese Egyptian adolescent girls Maced J Med Sci. 2011;4:17-24.
- World Health Organization. CHOosing Interventions that are Cost Effective (WHO-CHOICE): Cost-effectiveness thresholds. Geneva: World Health Organization; 2005 [cited 2011 3rd April]; Available from: http://www.who.int/choice/costs/CER_thresholds/en/index.html.
- Salize HJ, Merkel S, Reinhard I, et al. Cost-effective primary care-based strategies to improve smoking cessation: more value for money. Arch Intern Med. 2009 February 9, 2009;169:230-5.
- Sevick MA, Dunn AL, Morrow MS, et al. Cost-effectiveness of lifestyle and structured exercise interventions in sedentary adults: Results of project ACTIVE. Am J Prev Med. [doi: DOI: 10.1016/S0749-3797(00)00154-9]. 2000;19:1-8.
- Sevick MA, Napolitano MA, Papandonatos GD, et al. Cost-effectiveness of alternative approaches for motivating activity in sedentary adults: results of Project STRIDE. Prev Med. 2007;45:54-61.
- Salkeld G, Phongsavan P, Oldenburg B, et al. The cost-effectiveness of a cardiovascular risk reduction program in general practice. Health Policy 1997;41(2):105-19.
- Bertera RL. The effects of workplace health promotion on absenteeism and employment costs in a large industrial population. Am J Public Health. 1990;80(9):1101-5.
- Aldana SG, Merrill RM, Price K, et al. Financial impact of a comprehensive multisite workplace health promotion program. Prev Med. 2005;40:131-7.
Please cite this article as:
Siow Yen Liau, Asrul A Shafie, Mohamed Azmi A Hassali and Mohamed Izham Mohamed Ibrahim, Cost-Effectiveness Analysis of a Behavioral Risk Factor Reduction Program at a Worksite: Experience From a Public University in Malaysia. Malaysian Journal of Pharmacy (MJP). 2014;11(1):6-18. https://mjpharm.org/cost-effectiveness-analysis-of-a-behavioral-risk-factor-reduction-program-at-a-worksite-experience-from-a-public-university-in-malaysia/