Abstract
Study was conducted to investigate the influences of patient-related factors in diabetic management among non-insulin-treated type 2 diabetics in Outpatient Department, Hospital Kemaman. Convenience interview has been conducted, followed by further review of outpatient cards. Data collected from 29 subjects was analyzed by using SPSS Version 11. The inclusive criteria were patients diagnosed with diabetes for at least one year and on oral hypoglycemic agent. Patients on insulin treatment were excluded. The efficacy parameter was the fasting blood glucose level. 86.2% of study population were non-smokers. 41.4% consumed alternative medicines concurrently with antidiabetic medications. Majority of the subjects practiced lifestyle modifications, 62.1% in the form of routine exercise and 79.3% dietary modifications. 24.1% and 20.7% received counseling before being put on diabetic medications and on lifestyle modifications respectively. Many diabetics have poor understanding on their medications. Only 27.6% have their fasting blood glucose level ≤ 7mmol/L during the study duration. 72.4% patients claimed to have good compliance to the medications prescribed. Study revealed that patients had better glycaemic control if they had better understanding/knowledge about the medications, had better compliance, practice lifestyle modifications and had been counseled before. Other variables (age, smoking and concurrent use of alternative medicines) failed to demonstrate significant effect on glycaemic control. This study revealed problems such as non-optimal glycaemic control, insufficient patients’ knowledge about the disease and medications, and inadequate compliance in diabetic population. Pharmacists can help the community to manage diabetes better. This information is expected to be useful for pharmacists in improving their roles.
Introduction
Diabetes is a worldwide common chronic disorder. In ASEAN region, it is estimated that 7 million people are affected by diabetes mellitus [1]. In Malaysia, diabetes is one of the most prevalent chronic illnesses which contribute to ill health and premature mortality. The prevalence is about 8% [2]. Diabetes occurs when the pancreas fails to produce adequate insulin or when the body cannot utilize the insulin effectively (insulin resistance). It is a syndrome characterized by hyperglycaemia together with other metabolic abnormalities (e.g. disturbance in lipid and protein metabolism).
Essentially, diabetes mellitus is categorized into 2 groups: type 1 diabetes and type 2 diabetes. According to American Diabetes Association (ADA), 90-95% of patients diagnosed with diabetes are type 2 [3].
Type 2 Diabetes Mellitus
Type 2 diabetes is also known as adult-onset diabetes due to its relatively late onset compare with type 1 diabetes. The disorder occurs as a result of impaired insulin secretion; tissue resistance to insulin or due to increase hepatic glucose output. The long-term consequences of diabetes account for the majority
of morbidity and mortality. Chronic sequelaes of diabetes always link with poor diabetes control. Glucose toxicity as a result of uncontrolled hyperglycemia appears to contribute to the development and progression of microvascular complications (retinopathy, nephropathy and neuropathy). Diabetes is also the risk factor for macrovascular implications (e.g. cardiovascular, cerebral vascular and peripheral vascular systems). [4]
Currently there is no known cure for diabetes but the disease can be controlled enabling the patient to lead a healthy and productive life. The primary goal of diabetes management is to bring the glucose level as close to normal value as possible. There are five major components in the management of diabetes mellitus: diet, exercise, education, oral hypoglycemic agents and insulin. In addition, monitoring of glycaemic control and management of complications should also be emphasized. Good glycaemic control prevents/delays short term as well as the long term diabetic complications.
Objectives
General objectives
- To investigate the influence of patient-related factors in diabetes management in non-insulin- treated type 2 diabetics (in outpatient department of the Hospital Kemaman).
- To analyze and determine factors which might affect the glycaemic control.
Specific objectives
- To determine patients’ understanding/ knowledge towards oral hypoglycaemic agents in non-insulin treated type 2 diabetics.
- To investigate the patients’ compliance to the diabetes control.
- To analyze the roles of lifestyle modifications on diabetes management.
- To investigate the roles of counseling on diabetes management.
- To identify the barriers towards effective glycaemic control and steps to overcome the barriers.
- To recognize pharmacists roles in improving glucose management in diabetic patients.
Definition
a) Diabetes mellitus
In practice, diagnosis of diabetes mellitus must be confirmed by the measurement of venous plasma glucose. Malaysian Clinical Practice Guidelines stated that the diagnosis value of diabetes is as follow:
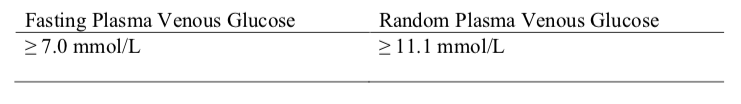
In asymptomatic patient, 2 abnormal glucose values are required to confirm the diagnosis of diabetes whereas for patient presents with symptom(s), only one abnormal glucose value is diagnostic.[5]
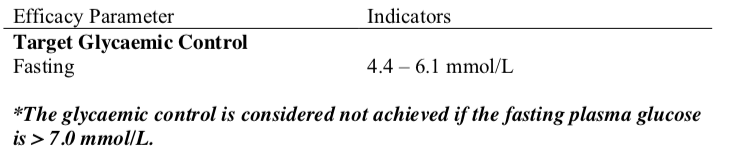
b) Efficacy Parameter of Glycaemic Control
Many quality indicators have been proposed to measure different aspects of diabetes management. In this study, the efficacy parameter used is the fasting blood glucose level.
c) Understanding / Knowledge of Medications Taken
Patients’ knowledge of the medications taken (oral hypoglycemic agents, OHA) is expected to be one of the factors affecting glycaemic control. In this study, several questions regarding medications taken had been forwarded to the patients to assess their understanding about the oral hypoglycaemic agents consumed.
Below are some of the questions asked:
Understanding / Knowledge of Medication Name | – Do you know the name (Brand Name / Generic Name) of the medications taken? – How do you recognize your medications? |
| Understanding / Knowledge of Medication Indications | – What this particular medication is indicated for? – How this OHA agent acts on the blood glucose level? |
| Understanding / Knowledge of Medication Dosage & Administration | – How is the medication(s) taken? Dose & frequency – Pre or post prandial? – What do you do when you miss a dose? |
| Understanding / Knowledge of Medications Storage | – Where do you keep your medicines? – What storage condition do you think might affect the medication’s efficacy? |
Each section counted for 1 mark:
| Level of understanding/ knowledge | Marks |
|---|---|
| Poor | 0-1 |
| Moderate | 2-3 |
| Good | 4 |
d) Compliance
Type 2 diabetic patients usually were on oral hypoglycaemic agent(s) either on mono- or poly- therapy. Patients have to take their medication(s) in multiple daily dosing in order to achieve good glycaemic control. Compliance to medications, therefore, plays an essential role to ensure blood glucose level is well-controlled. In this study, 6 following questions were asked to evaluate the compliance. Each question counted for 1 mark.
- How are the medications taken?
- Have you ever forgotten to take your medications? How often?
- How frequent are you delayed in taking daily medications?
- What do you do when you miss a dose?
- When do you come for follow up / refill?
- Do you share the medications with some one else?
The interviewer would then categorize patients into poor, moderate or good compliance based on the patient’s score.
| Level of compliance | Marks |
|---|---|
| Poor | 0-2 |
| Moderate | 3-4 |
| Good | 5-6 |
Methodology
A descriptive study has been carried out between Jan – March 2007. Sample was selected via convenience sampling among patients who were on oral hypoglycemic agent(s). The data collection was performed in two stages. In the first stage, patients were interviewed and data were recorded in a data collection form specially designed for this study (Appendix). Subsequently, outpatient cards of the same patients were reviewed to complete information.
The data was subsequently analyzed by using SPSS Version 11. Descriptive data were presented in percentage and Pearson Correlation test was used to evaluate the relationship between the fasting plasma glucose and patient’s factors.
Inclusion criteria
- Patient is on at least one type of oral hypoglycemic agent.
Exclusion criteria
- Patient newly diagnosed with diabetes mellitus (less than 1 year).
- Patient on insulin treatment
Result and discussion
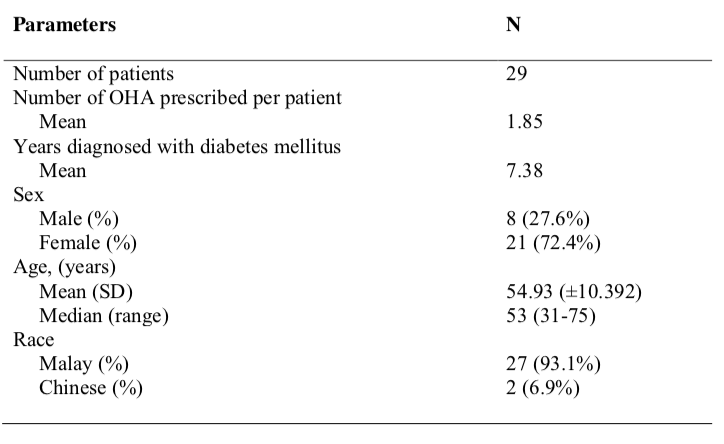
In this study, an overall of 29 patients with type 2 diabetes in outpatient department had been approached to assess the effect of several patient-related factors (which are expected to affect the body glycaemic control) on body blood glucose level. The study population consists of 27 (93.1%) Malays and 2 (6.9%) Chinese with 8 (27.6%) of the population were male and 21 54.93 ±10 and the mean of 7.38 years diagnosed with diabetes mellitus. [Table 1]
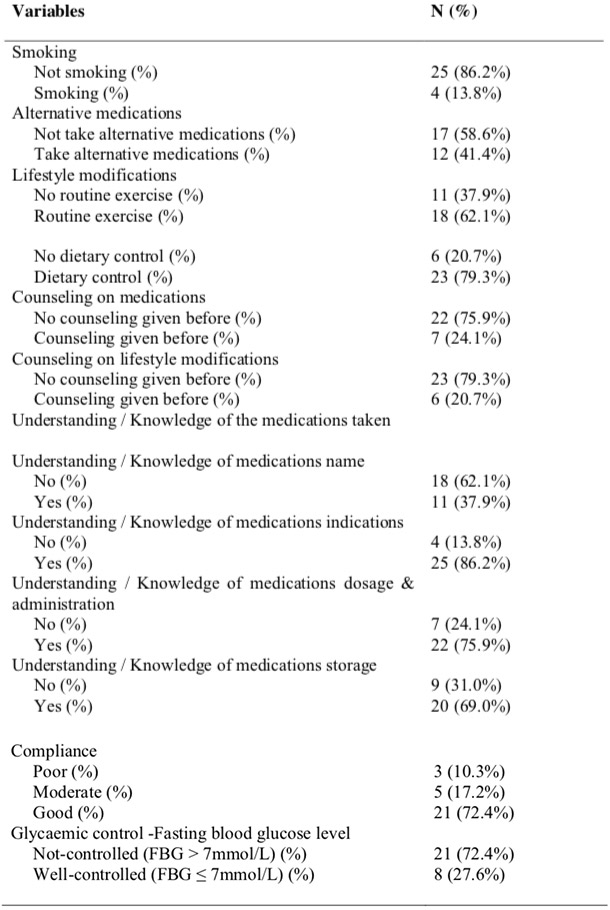
Most of the patients were non- smokers (86.2%). 41.4% of the population consumed alternative medications concurrently with antidiabetic medications. Lifestyle modifications, as part of diabetes management, practiced by majority of the population, with 62.1% patients claimed exercise routinely and 79.3% patients controlled their daily dietary intake.
Approximately one quarter of the population received counseling on diabetes prior to the study (24.1% and 20.7% patients received counseling before being put on diabetic medications and lifestyle modifications respectively). There are many patients out there who still do not completely understand about the medications prescribed to them. Good glycaemic control is the primary goal in diabetes management. The results, nevertheless, demonstrated a non- optimal control of blood glucose level. Only 27.6% have their fasting blood glucose level ≤7mmol/L during the study duration. More than 70% (72.4%) patients claimed to have good compliance to the medications prescribed. Some patients acknowledge moderate-poor compliance due to personal disability, old age, multiple drug regimen and other problems. Table 2 listed the variables that might affect the glycaemic control.
Patient-related factors have always been identified as the determining factors towards good glycaemic control. Gycaemic control, therefore, is expected to be improved if these determining factors are improved. It is expected that blood glucose level might achieve well-controlled level if the following criteria are met:
- younger age (expected to be more aware of the importance of self-care and have better understanding about the medications taken)
- non-smoker
- has better understanding about the medications taken
- has good compliance to the medications taken
- counseling on medications and lifestyle modifications given before being put on diabetic medication(s)
- practices lifestyle modifications, involving dietary control and routine involvement in physical exercise
Concurrent use of alternative medicine is also expected to influence the diabetic control.
Table 3 showed the correlation between the patient’s factors and the fasting plasma glucose. The results revealed that fasting blood glucose level had no significant correlation with patients’ age. Positive correlations found to be established between fasting blood glucose level and patients’ understanding / knowledge towards oral hypoglycaemic agents. Patients had their blood glucose level better controlled when they had higher knowledge of the indications, dosage & administration and storage of the medications. Patients’ knowledge about the name of the medications, however, did not improve the glycaemic control significantly.

Study also showed that better medication compliance produced better glycaemic control. This result was parallel with the findings from Duff EM; O’Connor A and friends stating that there was an inverse relationship between self-care scores and HbA1c% (6). In Duff’s study, self-care practices included weight control, exercise and medication compliance.
Lifestyle modifications including routine exercise and dietary control appeared to influence the fasting blood glucose level positively. Patients who practiced lifestyle modifications were found to have better glycaemic control. The parallel results was demonstrated by Sone H ; Katagiri A and friends who concluded that lifestyle modification had a small but significant improving effect on glycaemic control [7].
In addition, this study found that the relationship between counseling given before and the extent of glycaemic control. It was found that patients who had been counseled before whether on lifestyle modifications or medications or both presented with better blood glucose
control. This finding was corresponded to the finding by Kirk A and friends.(8) The researchers concluded that physical activity counseling was effective in promoting physical activity in people with Type 2 diabetes. The counseling improved glycaemic control in these patients. One of the problems highlighted here is that only a minority of the population has been counseled before and has sufficient knowledge about the disease and medications taken. Counseling will help patients understand the management of diabetes better and therefore, improve the compliance and glycemic control.
It was found that no significant correlation between smoking and fasting blood glucose levels. In other words, there was no significant difference in glycaemic control between smoker and non-smoker. However the expectation that non- smokers would have better blood glucose control, can not be confirmed in this study due to the limitation in sample size. Only 4 out of 29 in the study population were smokers.
The study also failed to demonstrate any correlation between the consumption of alternative medications and the fasting blood glucose level. About half of the study populations (41.4%) were taking alternative medicines concurrently with oral
hypoglycaemic agents with the beliefs that the alternative approaches will aid in their glycaemic control. Akar kayu, pegaga and traditional medicines were among those taken by these patients. The beliefs that the consumption of alternative medication helps in the management of glycaemic control, however, was not confirmed in this study. The role of alternative medicines in diabetes control is still under investigation. Not much established clinical data is available for alternative medicines use. Larger-scale and more comprehensive study on the use of alternative medicines in diabetes management should be carried out in the future.
This study managed to demonstrate some significant results but the correlations were not that impressive (correlation coefficient values were small). Diabetes is a progressive condition in which β-cell function deteriorates with increasing duration of diabetes. Stepwise therapy with multiple pharmacological therapies, therefore, is often needed over time to maintain target glucose control. Intermittent uncontrolled blood glucose level is not a definite indicator for poor diabetic control. It might just reflect a further progression of the disease and a more aggressive treatment is needed. Improving patients’ factors, of course, will slow down the disease progression but persistent good glycaemic control requires a combination of many factors. In this study, the analysis only involved the correlation between each single variable with blood glucose level.
Limitation of the study
The study has several limitations such as small sample size (N=29) and the finding does not reflect the overall situation in the diabetes population. Secondly, most of the data were gathered though verbal communications with patients (compliance, alternative medications, understanding about medications given, previous counseling history and complications). This technique is prone to possibility of incomplete or bias data. Thirdly, the study uses an average of 2 readings of fasting blood glucose that were taken within 3 months. Few readings within short period of time-frame might influence the average of blood glucose value. Finally the study does not use HbA1c level although HbA1c is a better indicator of glycaemic control. HbA1c is not routinely done at the studied hospital.
Recommendation
Education and counseling on medications and lifestyle modifications should be initiated at diagnosis stage and reinforced regularly. Group counseling can be conducted from time to time and patients are highly encouraged to participate in group counseling. Through group counseling, patients can share their problems in daily diabetes management, understand more about the disease and be able to manage the disease better.
Further study using larger population can be conducted to survey the effect of a combination of multiple factors in diabetic control. Future study is recommended to use HbA1c level as efficacy parameter for a more reliable result.
References
- Wild S, Roglic G, Green A, Sicree R, King H. Global prevalence of diabetes: estimates for the year 2000 and projections for 2030. Diabetes Care 2004;27:1047-53.
- National Health & Morbidity Survey 2, 1996.
- American Diabetes Association. Standards of medical care in diabetes. Diabetes Care 2006;29:S4-42
- Mary Anne Koda-Kimble, Lloyd Yee Young, Wayne A.Kradjan & B.Joseph, Applied Therapeutics: The Clinical Use of Drugs, 7th Edition, 2001, Lippincott Williams & Wilkins.
- Ministry of Health Malaysia, Persatuan Diabetes Malaysia, Academy of Medicine. Clinical Practice Guidelines – Management of Type 2 Diabetes Mellitus, Third edition, 2004.
- Duff EM; O’Connor A; McFarlane-Anderson N; Wint YB; Bailey EY; Wright- Pascoe RA, The University of the West Indies School of Nursing, Mona, Kingston 7, Jamaica, Self-care, compliance and glycaemic control in Jamaican adults with diabetes mellitus, 2006.
- Sone H; Katagiri A; Ishibashi S; Abe R; Saito Y; Murase T; Yam ashita H; YajimaY; Ito H; Ohash i Y; Akanuma Y; Yamada N; Ef fects of lifestyle modifications on patients with type 2 diabetes: the Japan Diabetes Complications Study (JDCS) study design, baseline analysis and three year-interim report, 2002.
- Kirk A ; Mutrie N ; MacIntyre P ; Fisher M, Centre for Exercise Science and Medicine, University of Glasgow, Scotland. Effects of a 12-month physical activity counselling intervention on glycaemic control and on the status of cardiovascular risk factors in people with Type 2 diabetes, 2004.
Please cite this article as:
Yap Li Swan, Influences of Patient-Related Factors in Diabetes Management Among Non- Insulin-Treated Type 2 Diabetics. Malaysian Journal of Pharmacy (MJP). 2008;6(1):256-267. https://mjpharm.org/influences-of-patient-related-factors-in-diabetes-management-among-non-insulin-treated-type-2-diabetics/