ABSTRACT
Introduction: The prevalence of mental health issues in Malaysia has tripled from 10.7 % in 1996 to 29.2 % in 2015. This was reflected by an increasing usage of psychotropic drugs over the past two decades. Thus, this study was carried out to explore the utilization trends of psychotropic drugs prescribed in Serdang Hospital. Method: This observational retrospective quantitative study was conducted using 11-year data from January 2008 to December 2018. Dispensing data was obtained using the electronic hospital information system (eHIS) in Serdang Hospital. Defined daily doses per 1000 populations per year metric (DDDs / 1000 / year) were used to compare the popularity of psychotropic classes and individual drugs. A comparison of the frequency and distribution of the drugs over time was made using Microsoft Office Excel 2013. Result: Total utilization of psychotropic drugs increased markedly by 859.2 % (from 75.9 to 727.8 DDDs / 1000 / year) from 2008 to 2018. Antidepressants were the most frequently dispensed class, with a significant increase by 1828.6 % (from 20 to 385.9 DDDs / 1000 / year). On the other hand, attention deficit hyperactivity disorder (ADHD) medication was the least dispensed class, from no usage in 2008 to 4.3 DDDs / 1000 / year in 2018. In 2018, out of 27 psychotropic drugs, sertraline (26.4 %) was the most frequently dispensed drug with 192.3 DDDs/1000/year. Conversely, clobazam (0.2 %) was the least dispensed drug with 1.2 DDDs / 1000 / year. Conclusion: Psychotropic drug utilization in Serdang Hospital increased markedly over the study period. All six classes contributed to the increment. Appropriate use of psychotropic drugs should be investigated in future.
INTRODUCTION
Psychiatric disorders are a growing public health concern worldwide. They affected more than 1 billion people globally in 2016 [1]. Approximately 80% arise from low and middle-income countries [2]. In Malaysia, the prevalence of psychiatric disorders among adults increased from 10.7 % in 1966, to 11.2 % in 2006, and to 29.2 % in 2015 [3]. Among all types of psychiatric disorders, depression was known to occur most commonly in Malaysia, affecting nearly 2.3 million people in Malaysia [4].
Psychiatric disorders cause significant burden on societies globally [5]. Approximately a third of those with major psychiatric disorders developed into long term disability and dependency [6]. The 2010 Global Burden of Disease study concluded that psychiatric disorders were the fifth leading cause of burden worldwide (equivalent to 7.4 % of all disability-adjusted life years (DALYs)) and the leading cause of disability (equivalent to 22.9 % of all years lived with disability (YLDs)) [7]. They also imposed additional burden associated with suicide and ischemic heart disease [8][9]. By the year 2030, it is predicted that the most burdening illness globally will be depression [10]. In Malaysia, psychiatric disorders accounted for 8.6 % of total DALYs in 2016 [11].
Psychotropic drugs remain a mainstay in the treatment of psychiatric disorders. Data from previous studies indicated increasing utilization of drugs for psychiatric disorders in different parts of the world over the past two decades [12][13][14][15][16][17][18][19]. This increase was also evident in the children and adolescent population [20][21]. In a developing country like Malaysia, a wide array of psychotropic drugs is available. With the development of newer drugs such as selective serotonin reuptake inhibitors (SSRIs) and atypical antipsychotics, more treatment options are available, including augmentation therapy with these newer drugs for patients with treatment-resistant psychiatric disorders. Various factors such as efficacy, safety, cost of drugs and local paradigms may change the drug prescribing habits, and thus affect the outcome. With this backdrop in mind, this study is conducted to investigate how the utilization trend of psychotropic drugs has been changing over time. Such understanding could yield invaluable insights which could be utilized for optimization of psychotropic drug prescribing patterns.
METHOD
This observational retrospective quantitative study was conducted using 11-year data from January 2008 to December 2018. This study was registered with the National Medical Research Register, Ministry of Health Malaysia (NMRR ID-NMRR-19-788-45961).
This study included data on oral psychotropic drugs dispensed in emergency pharmacy, in-patient pharmacy, out-patient pharmacy and ward floor stock. Data on patients from other Ministry of Health (MOH) facilities who were referred to Serdang Hospital solely for the collection of medication as well as medication loaned to other facilities were excluded from this study. Dispensing data was obtained using the electronic hospital information system (eHIS) in Serdang Hospital. Defined daily doses per 1000 populations per year metric (DDDs / 1000 / year) were used to compare the usage of psychotropic classes and individual drugs. A comparison of the frequency and distribution of the medications over time was made using Microsoft Office Excel 2013.
RESULT AND DISCUSSION
Overall dispensing for the six major classes of psychotropic drugs (anxiolytics and sedatives, antidementia, attention deficit hyperactivity disorder (ADHD) medication, mood stabilizers, antidepressants and antipsychotics) is shown in Figure I. When all the psychotropic classes were considered, the total DDDs / 1000 / year increased markedly by 859.2 % (from 75.9 to 727.8 DDDs / 1000 / year). This notable increase was driven by increases in all psychotropic classes, with antidepressants contributing the most increase by 1828.6% (from 20.01 to 385.92 DDDs / 1000 / year). This is because depression was the most widely treated psychiatric disease in Malaysia [4]. A previous study conducted in Australia also concluded that the increase in psychotropic dispensing was majorly driven by increases in antidepressants (95.3 %) [17].
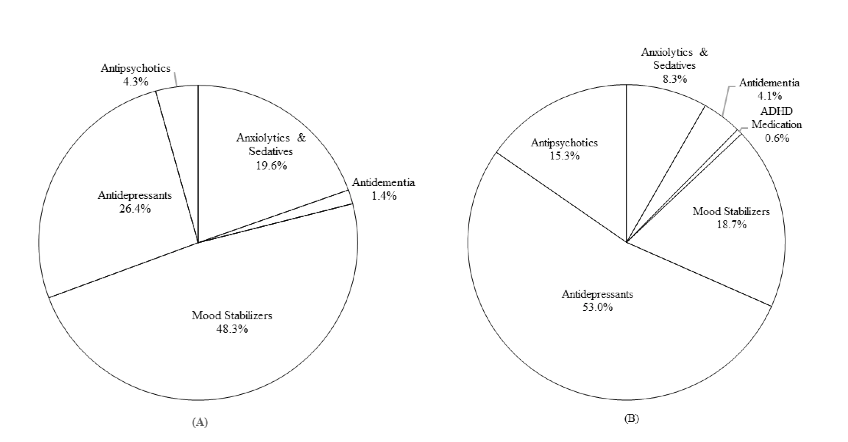
Comparison of the contribution of each psychotropic class to total psychotropic dispensing in 2008 and 2018 is shown in Figure II. Our findings illustrated that the most frequently dispensed class was mood stabilizers (48.3 %) in 2008 and antidepressants (53 %) in 2018. This is in tune with data from several studies which reported that antidepressant were the most popular psychotropic class of late [15][17][22][23]. As for the least dispensed psychotropic class, our results revealed that ADHD medication was the least dispensed in 2008 (no usage) and 2018 (0.6 %). This may be attributable to the reluctance of parents to allow their children to take medications for long term [16]. Parents are concerned about their children’s treatment options. They believe that a prolonged use of stimulants can result in increased risk of drug addiction [24]. They also have the misconception that the cause of ADHD symptoms is associated with sugar intake, and thus they are not keen to start their children with medication as the first option [25].
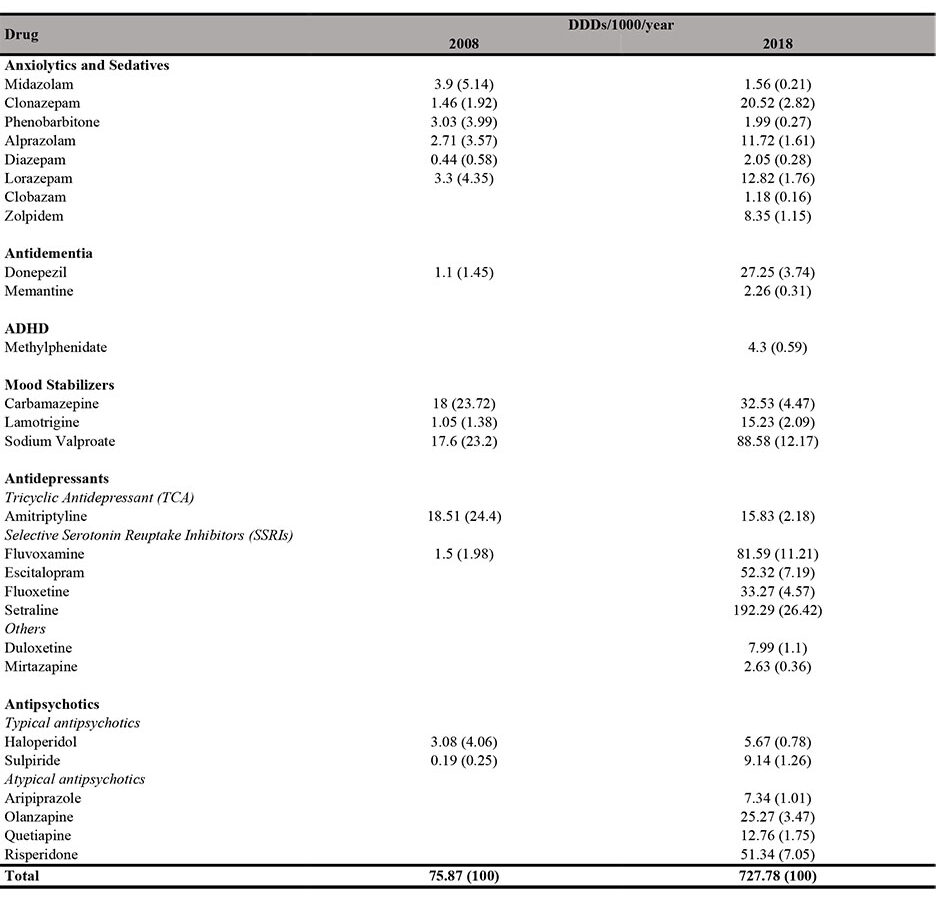
Comparison of the list of psychotropic drugs available in Serdang Hospital in 2008 and 2018 is shown in Table I. There were a number of new psychotropic drugs being added into the drug formulary, with 14 drugs in 2008 versus 27 drugs in 2018. This could explain the significant increase in drug utilization from 2008 to 2018 because these drugs are known to have clinical superiority relative to the first-generation drugs.
Of the 27 psychotropic drugs in 2018, sertraline (26.4 %) was the most popular dispensed drug with 192.3 DDDs / 1000 / year. In contrast, clobazam (0.2 %) was the least dispensed drug with 1.2 DDDs / 1000 / year. Data from the Malaysian Statistics on Medicines found a similar trend, which documented that sertraline was among the top three most dispensed drugs in public sectors in 2014, while clobazam was the least popular drug [16]. An overseas study conducted in Iran also reported that sertraline (12.4 %) was the most commonly used psychotropic drug between 2012 and 2013 [23].
Anxiolytics and sedatives
We observed a remarkable 305.6 % increase in anxiolytics and sedatives dispensing (from 14.8 to 60.2 DDDs / 1000 / year) from 2008 to 2018. However, our findings are in contrast to several recent local and global studies. Data from Malaysian Statistics on Medicines indicated a drop of 5.8 % in the overall usage of anxiolytics and sedatives from 2011 to 2014 [16]. An overseas study carried out in Australia found that dispensing of anxiolytics remained unchanged, while sedatives decreased by 26.4 % [17]. Hence, results of our study should raise awareness regarding appropriate prescribing practices for anxiolytics and sedatives. This includes strategies to discontinue long-term prescribing of benzodiazepine. Benzodiazepines are recommended to be tapered down slowly, with psychological support emphasized during the tapering process. Basic approaches include the use of the same medication for tapering, switching to a longer-acting equivalent and the use of adjunctive medications to mitigate the withdrawal symptoms. The recommended initial dose reduction ranges between 5 % and 25 % of the starting dose, followed by further reduction of 5 % to 25 % every one to four weeks as tolerated [26].

Of the 8 anxiolytics and sedatives, clonazepam was the most widely dispensed drug. Use of clonazepam increased markedly by 1305.5 % (from 1.46 to 20.52 DDDs / 1000 / year). The findings are consistent with several drug utilization studies conducted in tertiary care hospitals in India [27][28]. Benzodiazepines are known to have differences in distribution, elimination half-life and rate of absorption. Clonazepam is a long-acting and high-potency benzodiazepine, having lower lipid solubility and longer elimination half-life, as compared to lorazepam and alprazolam. Thus, it has a lower incidence of adverse events, drug abuse and interdose withdrawal symptoms [29]. Moreover, it has no drug interaction with antidepressants, and thus, favouring its use over other benzodiazepines [30][31].
Antidementia
Our study’s result showed that donepezil was the most preferred drug for dementia over memantine. According to the Malaysia Clinical Practice Guidelines on Management of Dementia, donepezil has been approved for mild to severe dementia. As for memantine, it is approved to be used only for moderately severe to severe dementia and in patients who are unable to tolerate acetylcholinesterase inhibitors such as donepezil [32].
ADHD medication
Our study revealed that methylphenidate was the only psychiatrist-prescribed stimulant for the treatment of ADHD in children. A study conducted in Iran also reported similar practice in ADHD prescription [23]. In terms of drug efficacy, it reduces core symptoms of ADHD such as poor concentration and hyperactivity by 70 % as compared to placebo [33]. It is being recommended by the National Institute for Health and Clinical Excellence (NICE), the Scottish Intercollegiate Guidelines Network (SIGN) and the American Academy of Pediatrics (AAP) as the first line drug in treating ADHD [34][35][36]. In terms of drug safety, it generally has a favourable side effect profile which is mild and of short duration. The most common side effect is appetite suppression which can be overcome by taking the drug after meal.
Mood stabilizers
Our study showed that the drugs used in the treatment of bipolar disorders consist of anticonvulsant drugs only, namely sodium valproate, carbamazepine and lamotrigine. Anticonvulsants exhibit their acute antimanic response and prophylactic efficacy in bipolar disorders in various ways, which include blockage of the voltage-gated ion channels (sodium valproate, carbamazepine and lamotrigine), enhancement of gamma aminobutyric acid (GABA) inhibition (sodium valproate), and reduction of glutamate release (lamotrigine) [37]. Their role in the treatment of bipolar disorders was evident in many recent studies despite lithium being the mainstay of treatment for many years [38]. This is because lithium has a narrow therapeutic index of safety, thus requiring frequent blood monitoring as per recommendations by the National Patient Safety Agency [39]. In Serdang Hospital, the lithium blood monitoring test is not available, therefore discouraging its use for bipolar disorders.
Among the anticonvulsants, sodium valproate was the most commonly dispensed mood stabilizer, which is in line with the findings from several overseas studies [18][27]. It has been recommended as the first line drug for bipolar patients because it demonstrates efficacy in the treatment of a broad spectrum of bipolar conditions, including as augmentation therapy in schizophrenia, as augmentation with SSRI in depression, organic brain syndrome and dementia with behavioural symptoms [40][41].
Antidepressants
Our results showed that the use of SSRIs spiked notably, while tricyclic antidepressants (TCAs) dropped gradually over the study period. This finding is comparable to both local and overseas studies in which SSRIs were the preferred prescribed antidepressant class [13][17][18][19][42]. Considering efficacy and safety profiles, SSRIs are recommended as the initial treatment of depression, while conventional antidepressants (TCAs) are considered as second line treatment [43]. SSRIs have high affinity to serotonin reuptake receptors but little blocking activities at the histaminic, cholinergic, and alpha-adrenergic receptors. For these reasons, they have a superior safety profile relative to TCAs.
Our study showed that sertraline was the most widely used SSRI drug. This finding is in agreement with several similar studies done in other countries [17][44]. One of the reasons is that, sertraline has the most favourable balance between effectiveness, side effects, and cost [45]. It only produces mild inhibition on cytochrome P450 2D6 and has little effect on other cytochrome P450 isoenyzmes as compared to other SSRIs. Therefore, in patients at risk for drug interactions, sertraline is considered as a first line treatment option [46][47]. Additionally, it is relatively safe in overdose [47].
Antipsychotics
Our findings showed a paradigm shift from typical antipsychotics to atypical antipsychotics. In 2008, only typical antipsychotics were used for treatment of schizophrenia. However, over the years, there was a surge in atypical antipsychotics usage, overtaking typical drugs. This finding is in tune with several drug utilization studies [14][17][28]. This may be explained by their role in the treatment of negative symptoms, lesser extrapyramidal side effects and lower treatment discontinuation rate [48]. Besides, they have been used as adjunctive therapy to mood stabilizers, providing faster and more notable symptom improvement compared to conventional monotherapy with mood stabilizer [49].
Our results reported that risperidone was the most preferred antipsychotics, with a tremendous rise by 3300% (from 1.51 to 51.34 DDDs / 1000 / year) from 2009 to 2018. This is significantly higher when compared to data from the Malaysian Statistics on Medicines, which reported 34.3% increase from 2011 to 2014 [16]. Risperidone was extensively prescribed most likely because it is the only atypical antipsychotic drug with prescriber category B as listed in the MOH drug formulary. All medical officers, including consultants and specialists, can start patients on this drug when indicated. In terms of weight gain and metabolic abnormalities, it is better tolerated than olanzapine and quetiapine [50].
CONCLUSION
Psychotropic dispensing in Serdang Hospital increased markedly from 2008 to 2018, with major increases contributed by antidepressant use. Growing increase in anxiolytics and sedatives usage should raise awareness on appropriate benzodiazepine prescribing. The inclusion of newer drugs such as SSRIs and atypical antipsychotics has altered the treatment paradigms.
ACKNOWLEDGEMENT
We would like to thank the Director General of Health Malaysia for his permission to publish this report. We also would like to express our sincere gratitude to our advisor, Dr Wardati binti Mazlan Kepli and everyone who has been involved directly or indirectly in helping us to complete this study.
CONFLICT OF INTEREST
This study has no conflict of interest. This research did not receive any specific grant from funding agencies in public, commercial or not-for-profit sectors.
REFERENCE
- Rehm J, Shield KD. Global burden of disease and the impact of mental and addictive disorders. Current Psychiatry Reports. 2019; 21(2): 10. https://doi.org/10.1007/s11920-019-0997-0
- Jacob K, Patel V. Classification of mental disorders: a global mental health perspective. The Lancet. 2014; 383(9926): 1433-1435. https://doi.org/10.1016/S0140-6736(13)62382-X
- Institute for Public Health, Ministry of Health Malaysia. National health and morbidity survey 2015 vol. 2: non-communicable diseases, risk factors and other health problems [Internet]. 2015 [cited 2021 Jan3]http://iku.moh.gov.my/images/IKU/Document/REPORT/nhmsreport2015vol2.pdf
- Mukhtar F, Oei TP. A review on the prevalence of depression in Malaysia. Current Psychiatry Reviews. 2011; 7(3): 234-238. https://doi.org/10.2174/157340011797183201
- Benziger CP, Roth GA, Moran AE. The global burden of disease study and the preventable burden of NCD. Global Heart. 2016; 11(4): 393-397. https://doi.org/10.1016/j.gheart.2016.10.024
- Mathers CD, Loncar D. Projections of global mortality and burden of disease from 2002 to 2030. PLoS Medicine. 2006; 3(11): e442. https://doi.org/10.1371/journal.pmed.0030442
- Whiteford HA, Degenhardt L, Rehm J, Baxter AJ, Ferrari AJ, Erskine HE, et al. Global burden of disease attributable to mental and substance use disorders: findings from the global burden of disease study 2010. The Lancet. 2013; 382(9904): 1575-1586. https://doi.org/10.1016/S0140-6736(13)61611-6
- Byass P, de Courten M, Graham WJ, Laflamme L, McCaw-Binns A, Sankoh OA, et al. Reflections on the global burden of disease 2010 estimates. PLoS Medicine. 2013; 10(7): e1001477. https://doi.org/10.1371/journal.pmed.1001477
- Ferrari AJ, Charlson FJ, Norman RE, Patten SB, Freedman G, Murray CJ, et al. Burden of depressive disorders by country, sex, age, and year: findings from the global burden of disease study 2010. PLoS Medicine. 2013; 10(11): e1001547. https://doi.org/10.1371/journal.pmed.1001547
- World Health Organization. The global burden of disease: 2004 update [Internet]. 2008 [cited 2021 Jan 3]. Available from: https://www.who.int/healthinfo/global_burden_disease/GBD_report_2004update_full.pdf?ua=1
- Malaysian Healthcare Performance Unit, Ministry of Health Malaysia. Malaysian mental healthcare performance: technical report 2016. 2017 [cited 2021 Jan 12]. https://www.moh.gov.my/index.php/pages/view/971?mid=55
- Alexander GC, Gallagher SA, Mascola A, Moloney RM, Stafford RS. Increasing off-label use of antipsychotic medications in the United States, 1995-2008. Pharmacoepidemiology and Drug Safety. 2011; 20(2): 177-184. https://doi.org/10.1002/pds.2082
- Amuthaganesh M, Suhasinee S, Mathialagan S. Pattern of antidepressant utilization at a tertiary hospital in Malaysia (2009-2011). 2nd International Conference on Advances in Biotechnology and Pharmaceutical Sciences (ICABPS 2012); June 30-July 1, 2012; Bali. pp. 1-9.
- Ilyas S, Moncrieff J. Trends in prescriptions and costs of drugs for mental disorders in England, 1998–2010. British Journal of Psychiatry. 2012; 200(5): 393-398. https://doi.org/10.1192/bjp.bp.111.104257
- Olfson M, Marcus SC. National patterns in antidepressant medication treatment. Archives of General Psychiatry. 2009; 66(8): 848-856. https://doi.org/10.1001/archgenpsychiatry.2009.81
- Pharmaceutical Services Divison, Ministry of Health Malaysia. Malaysian statistics on medicine 2011–2014 [Internet]. 2017 [cited 2021Jan 3]. https://www.pharmacy.gov.my/v2/sites/default/files/document-upload/malaysian-statistics-medicines-2011-2014.pdf
- Stephenson CP, Karanges E, McGregor IS. Trends in the utilisation of psychotropic medications in Australia from 2000 to 2011. Australian & New Zealand Journal of Psychiatry. 2012; 47(1): 74-87. https://doi.org/10.1177/0004867412466595
- Walpoth-Niederwanger M, Kemmler G, Grunze H, Wei U, Hörtnagl C, Strauss R, et al. Treatment patterns in inpatients with bipolar disorder at a psychiatric university hospital over a 9-year period. International Clinical Psychopharmacology. 2012; 27(5): 256-266. https://doi.org/10.1097/YIC.0b013e328356ac92
- Yu Z, Zhang J, Zheng Y, Yu L. Trends in antidepressant use and expenditure in six major cities in China from 2013 to 2018. Front Psychiatry. 2020;11:551. https://doi.org/10.3389/fpsyt.2020.00551
- Karanges EA, Stephenson CP, McGregor IS. Longitudinal trends in the dispensing of psychotropic medications in Australia from 2009–2012: focus on children, adolescents and prescriber specialty. Australian & New Zealand Journal of Psychiatry. 2014; 48(10): 917-931. https://doi.org/10.1177/0004867414538675
- Kalverdijk LJ, Bachmann CJ, Aagaard L, Burcu M, Glaeske G, Hoffmann F, et al. A multi-national comparison of antipsychotic drug use in children and adolescents, 2005–2012. Child and Adolescent Psychiatry and Mental Health. 2017; 11(1): 55. https://doi.org/10.1186/s13034-017-0192-1
- Bagewadi H, Huded C. A study of prescription patterns of psychotropic medications in psychiatric outpatient department in a tertiary care center in North Karnataka. National Journal of Physiology, Pharmacy and Pharmacology. 2019; 9(12): 1221-1224. https://doi.org/10.5455/njppp.2019.9.0829705102019
- Sabahi A, Sepehri G, Mohsenbeigi M, Sepehri E. Patterns of psychotropic medication prescriptions by psychiatrists for private clinic outpatients in Kerman province, Iran. Sultan Qaboos University Medical Journal. 2014; 14(3): e382-e387.
- Robbins T. ADHD and addiction. Nat Med. 2002; 8(1): 24-25. https://doi.org/10.1038/nm0102-24
- Del-Ponte B, Anselmi L, Assuncao MCF, Tovo-Rodrigues L, Munhoz TN, Matijasevich A, et al. Sugar consumption and attention-deficit/hyperactivity disorder (ADHD): a birth cohort study. J Affect Disord. 2019; 243: 290-296. https://doi.org/10.1016/j.jad.2018.09.051
- National Center for PTSD. Effective treatments for PTSD: helping patients taper from benzodiazepines. 2015 [cited 2021 Jan 20]. https://www.ptsd.va.gov/publications/print/index.asp
- Chawla S, Agarwal M, Sharma S, Jiloha RC. Drug utilization study of psychotropic drugs among psychiatric outpatients in a tertiary care hospital. Indian Journal of Pharmaceutical Sciences. 2017; 79(6): 1008-1013. https://doi.org/10.4172/pharmaceutical-sciences.1000319
- Sabu L, Yacob M, Mamatha K, Singh H. Drug utilization pattern of psychotropic drugs in psychiatric outpatient department in a tertiary care teaching hospital. Asian Journal of Pharmaceutical and Clinical Research. 2017; 10(1): 259-261. https://doi.org/10.22159/ajpcr.2017.v10i1.15112
- Wang SM, Kim JB, Sakong JK, Suh HS, Oh KS, Woo JM, et al. The efficacy and safety of clonazepam in patients with anxiety disorder taking newer antidepressants: a multicenter naturalistic study. Clinical Psychopharmacology and Neuroscience. 2016; 14(2): 177-183. https://doi.org/10.9758/cpn.2016.14.2.177
- Martin P. Coadministration benzodiazepine and antidepressant drugs: the state of art. Encephale. 2006; 32(5): 753-766. https://doi.org/10.1016/s0013-7006(06)76228-5
- Nardi AE, Machado S, Almada LF, Paes F, Silva AC, Marques RJ, et al. Clonazepam for the treatment of panic disorder. Current Drug Targets. 2013; 14(3): 353-364. https://doi.org/10.2174/1389450111314030007
- Health Technology Assessment Section, Ministry of Health Malaysia. Clinical practice guidelines: management of dementia second edition [Internet]. 2009 [cited 2021 Jan 3]. https://www.moh.gov.my/moh/attachments/4484.pdf
- Schachter HM, Pham B, King J, Langford S, Moher D. How efficacious and safe is short-acting methylphenidate for the treatment of attention-deficit disorder in children and adolescents: a meta-analysis. Canadian Medical Association Journal. 2001; 165(11): 1475-1488.
- National Institute for Health and Clinical Excellence. Attention deficit hyperactivity disorder: diagnosis and management (NG87) [Internet]. 2018. https://www.nice.org.uk/guidance/ng87/resources/attention-deficit-hyperactivity-disorder-diagnosis-and-management-pdf-1837699732933
- Scottish Intercollegiate Guidelines Network. Management of attention deficit and hyperkinetic disorders in children and young people: a national clinical guideline (112) [Internet]. 2009 https://www.argyll-bute.gov.uk/sites/default/files/adhd_informtion.pdf
- American Academy of Pediatrics (AAP), Committee on Quality Improvement SoA-DHD. Clinical practice guideline: diagnosis and evaluation of the child with attention-deficit/hyperactivity disorder. Pediatrics. 2000; 105(5): 1158-1170. https://doi.org/10.1542/peds.105.5.1158
- Greenhill SD, Jones RS. Diverse antiepileptic drugs increase the ratio of background synaptic inhibition to excitation and decrease neuronal excitability in neurones of the rat entorhinal cortex in vitro. Neuroscience. 2010; 167(2): 456-474. https://doi.org/10.1016/j.neuroscience.2010.02.021
- Leo RJ, Narendran R. Anticonvulsant use in the treatment of bipolar disorder. a primer for primary care physicians. Primary Care Companion to the Journal of Clinical Psychiatry. 1999; 1(3): 74-84. https://www.psychiatrist.com/read-pdf/23828/
- Pharmaceutical Services Negotiating Committee. NPSA patient safety alert: safer lithium therapy [Internet]. 2009 [cited 2021 Jan 2021]. http://archive.psnc.org.uk/news.php/638/npsa_patient_safety_alert_safer_lithium_therapy.html
- Ayano G. Bipolar disorders and valproate: pharmacokinetics, pharmacodynamics, therapeutic effects and indications of valproate: review of articles. Bipolar Disord. 2016; 2(2): 109. https://doi.org/10.4172/2472-1077.1000109
- Bowden C, Göğüş A, Grunze H, Häggström L, Rybakowski J, Vieta E. A 12-week, open, randomized trial comparing sodium valproate to lithium in patients with bipolar I disorder suffering from a manic episode. International Clinical Psychopharmacology. 2008; 23(5): 254-262. https://doi.org/10.1097/YIC.0b013e3282fd827c
- Dutta S, Kaul V, Beg MA, Sindhu S, Singh NK, Dutta S, et al. A psychotropic drug use study among depression patients attending private psychiatric practitioners of Dehradun, Uttarakhand. International Journal of Medical Science and Public Health. 2015; 4(5): 634-638. https://doi.org/10.5455/ijmsph.2015.19012015129
- Malaysian Health Technology Assessment Section, Ministry of Health Malaysia. Clinical practice guidelines: management of major depressive disorder second edition [Internet]. 2019 [cited 2021 Jan 3]. https://www.moh.gov.my/moh/resources/Penerbitan/CPG/1)_CPG_Management_Major_Depressive_Disorder_(Second_Edition).pdf
- Islam B, Shahriar I, Jannat T. Prescribing pattern of antidepressant drugs in two teaching hospitals in Bangladesh. Mediscope. 2019; 6(2): 53-58. https://doi.org/10.3329/mediscope.v6i2.43153
- Cipriani A, Furukawa TA, Salanti G, Geddes JR, Higgins JP, Churchill R, et al. Comparative efficacy and acceptability of 12 new-generation antidepressants: a multiple-treatments meta-analysis. The Lancet. 2009; 373(9665): 746-758. https://doi.org/10.1016/S0140-6736(09)60046-5
- Hemeryck A, Belpaire FM. Selective serotonin reuptake inhibitors and cytochrome p-450 mediated drug-drug interactions: an update. Current Drug Metabolism. 2002; 3(1): 13-37. https://doi.org/10.2174/1389200023338017
- MacQueen G, Born L, Steiner M. The selective serotonin reuptake inhibitor sertraline: Its profile and use in psychiatric disorders. CNS Drug Reviews. 2006; 7(1): 1-24. https://doi.org/10.1111/j.1527-3458.2001.tb00188.x
- Zhang JP, Gallego JA, Robinson DG, Malhotra AK, Kane JM, Correll CU. Efficacy and safety of individual second-generation vs. first-generation antipsychotics in first-episode psychosis: a systematic review and meta-analysis. International Journal of Neuropsychopharmacology. 2013; 16(6): 1205-1218. https://doi.org/10.1017/S1461145712001277
- Correll CU. The role of antipsychotics and mood stabilizers in the treatment of bipolar disorder. Journal of Psychopathology. 2011; 17(3): 341-351.
- Rummel-Kluge C, Komossa K, Schwarz S, Hunger H, Schmid F, Lobos CA, et al. Head-to-head comparisons of metabolic side effects of second generation antipsychotics in the treatment of schizophrenia: a systematic review and meta-analysis. Schizophrenia Research. 2010; 123(2-3): 225-233. https://doi.org/10.1016/j.schres.2010.07.012
Please cite this article as:
Pei Yean Soo, Atiqah Hanis Mustapa, Hui Peng Lim, Chen Yuan Lee and Wen Suen Goh, Trends in the Utilization of Psychotropic Drugs in Serdang Hospital. Malaysian Journal of Pharmacy (MJP). 2021;2(7):51-57. https://mjpharm.org/trends-in-the-utilization-of-psychotropic-drugs-in-serdang-hospital/