Abstract
Objective: This study aimed to determine the effectiveness of a pharmacist-led audit-and-feedback intervention in promoting the appropriate prescribing of third-generation cephalosporins and timely culture and sensitivity (C&S) testing in patients admitted to a neurosurgical ward. Method: This quasi-experimental study was conducted from July 2019 to August 2020 in a tertiary public hospital in Malaysia. In the pre-intervention phase, seventy patients who have received treatment with third-generation cephalosporins were examined by a ward pharmacist. The use of a cephalosporin was deemed to be appropriate only if it was in line with either the National Antimicrobial Guidelines 2019 or the recommendations made by the Antimicrobial Stewardship team. The availability of C&S test performed before the first dose of cephalosporin was also studied. As an intervention, the findings were presented and discussed in a 2-hour feedback session. Subsequently, the post-intervention audit was performed in the same manner as in the pre-intervention phase. The primary outcome measures were the proportion of cases with appropriate use of cephalosporin and timely C&S testing. The variables were analysed descriptively. Pearson’s chi-square test was used to assess the differences in appropriateness of antibiotics use and C&S testing, in the pre- and post-intervention cohorts. Result: Seventy cases were studied in the pre- and another seventy in post-intervention phases. The proportion of cases with appropriate use of third-generation cephalosporin increased significantly from 77.1% (54 / 70) to 95.8% (67 / 70) following the intervention (p = 0.001). The proportion of cases with a C&S test performed timely also increased significantly from 38.6% (27 / 70) to 58.6% (41 / 70) (p = 0.018). Conclusion: The pharmacist-led audit-and-feedback intervention was effective in improving the appropriateness of the prescribing of third-generation cephalosporins and timely culture and sensitivity testing, indicating the antimicrobial stewardship strategy had produced a positive outcome.
Introduction
Third-generation cephalosporins have broad spectrum of antimicrobial activities and are able to cross the blood-brain barrier. This gives rise to their high usage as the empirical treatment of neurosurgical complications [1][2], which is often linked to antimicrobial resistance in nosocomial pathogens [3]. As a result, the treatment options for infections caused by gram-negative bacteria have become limited [4].
In Asia, ceftriaxone is the most widely used third-generation cephalosporin, prescribed for 59.1% to 81.8% of hospitalized patients [5][6]. Most of the time, it was used as the empirical treatment [7], including in neurosurgical wards [8]. Cefoperazone / sulbactam came in second, mainly prescribed for those with sepsis [9].
In Malaysia, the cephalosporin usage reached 650 defined daily dose/ 1000 patient-days in 2016. Slightly less than 80% of the cases had cephalosporins used as the empirical treatment, 13.6% for microbiologically confirmed diseases and 5.7% as surgical prophylaxis [10]. However, the use of antibiotics in wards was commonly found to be inconsistent with the recommendations in the National Antimicrobial Guideline (NAG) [11]. Another study also related to the inappropriate antibiotic prescribing to growing antimicrobial resistance and mortality in hospitalized patients [12]. It is believed that the most effective way to combat antimicrobial resistance is through the rational use of antibiotics [13].
The Antimicrobial Stewardship (AMS) Program was launched by the Ministry of Health (MOH) to promote the appropriate prescribing of antibiotics in Malaysia. It is run by a multidisciplinary team in each hospital, which includes infectious disease physicians, clinical microbiologists and ward pharmacists [14]. One of the important activities of the AMS team is to perform audits and provide feedback [15], with the aim to correct the inappropriate practice in antibiotic use [16].
Together with the AMS program, the NAG was introduced to guide the prescribers in antibiotic use. In public health institutions in Malaysia, prescribers are expected to follow the recommendations of the NAG when it comes to antibiotic use. The adherence to the NAG could be evaluated in several aspects, including the drug selection, the regimen used, and the purpose of treatment. Meanwhile, the AMS team served as an important point of reference when a clinical condition is not able to capture by the NAG.
In the Raja Permaisuri Bainun Hospital located in northern Malaysia, the 38-bed neurosurgical ward recorded the highest usage of ceftriaxone, with a defined daily dose of 189.11 / 1000 bed days between January and June 2019. This study aimed to evaluate the effectiveness of an audit-and-feedback intervention in promoting the appropriate prescribing of third-generation cephalosporins and timely culture and sensitivity (C&S) testing among patients admitted to this ward.
Method
This was a quasi-experimental study conducted in Raja Permaisuri Bainun Hospital, a tertiary public hospital in the Perak state of Malaysia, from July 2019 until August 2020. The audit consisted of pre-intervention, feedback and post-intervention phases. The patients included were those who were admitted to the neurosurgical ward during the pre- and post-intervention of the audit and received treatment with one of the three commonly used third-generation cephalosporin (ceftriaxone, cefoperazone / sulbactam and ceftazidime). The sample size required in each phase was estimated based on a previous study, which reported that the proportions of prescriptions showing an appropriate use of empirical antibiotics were 61.7% and 83.8% before and after an intervention, respectively [15]. With a confidence level of 95% and a power of 80%, the calculated sample size for the pre- and post-intervention phases was 63. To account for 10% of cases with incomplete information, 70 cases were studied in both phases.
Pre-intervention phase (1st July – 31st October 2019)
A ward pharmacist, who was also the AMS pharmacist, collected data of patients treated with the third-generation cephalosporin between 1st July and 31st October 2019 during routine ward round prospectively. The data collection and assessment were conducted at the point when the first dose of a cephalosporin was administered prior to any interventions made by the ward pharmacist. The information gathered included the types of antibiotics, their dosage and frequency, duration and the diagnosis of patients. In this context, inappropriate prescribing referred to the use of a cephalosporin not in line with either the NAG or recommendations of the AMS team, in term of drug selection, dose and frequency; and treatment duration. In a case that a condition was not captured by the NAG, the prescribers were expected to seek advices from the AMS team. Also, the prescribers were expected to perform a C&S test right before the first dose of a cephalosporin was given.
Intervention phase (13th December 2019)
The audit findings were then presented in a 2-hour feedback session, in which all the cases of inappropriate prescribing were discussed. The feedback session was led by the hospital AMS team, which consisted of AMS pharmacists, clinical microbiologists and infectious disease physicians. The attendees included neurosurgeons and medical officers from the neurosurgical department. The audit feedback was presented by the ward AMS pharmacist and the discussion emphasized the need to use cephalosporins according to the recommendations of the NAG (Table I), as well as to perform C&S testing right before empirical treatment was initiated.
The neurosurgical team agreed to the above recommendations, with an exception given to the use of ceftriaxone at their discretion in patients who had a basilar skull fracture complicated with cerebrospinal fluid (CSF) leak.

Post-intervention phase (15th December 2019 – 31st August 2020
The post-intervention audit was performed in the same manner as in the pre-intervention phase. No staff change took place throughout the audit period. To minimize the Hawthorne effect [17], only the head of neurosurgical department was informed on the conduct of the audit. Only one ward pharmacist was involved in the data collection and assessment in order to ensure the internal reliability of the assessment.
The statistical analysis was performed using the SPSS for Windows (Version 20.0. Armonk, NY: IBM Corp). The categorical variables were described as frequencies and percentages, and continuous variables as mean with standard deviation (SD). The independent t-test was used to assess the differences in age and length of stay, while the Pearson’s chi- square tests was used to assess the differences in gender, clinical diagnosis, antibiotics use, events of readmission and mortality, total prescribing issues, C&S testing and type of treatment involved in pre- and post-intervention phase. The statistical significance of the test was indicated by a p-value < 0.05.
The ethics approval for this study was obtained from the Medical Research and Ethics Committee (MREC) under the MOH, Malaysia [(Registration number: NMRR-19-804-47375 (IIR), approval number: KKM/NIHSEC/P19-945(10).]
Result
A total of 140 cases were examined in the pre- and post- intervention phases, 70 cases in pre-intervention and 70 in post- intervention. No differences in the distributions of age (t = -0.037, p = 0.759) and gender (X2 = 0.150, p = 0.847) were observed between two phases. The clinical diagnoses between the two cohorts were significantly different (X2 = 20.376, p = 0.002). Presumed meningitis was the most common conditions in both cohorts, with 44 (62.9%) and 40 (57.2%) patients in the pre- and post-intervention phases, respectively. Hospital- acquired pneumonia was found to be more common in the pre- intervention phase (n = 6,8.6%), while more patients had brain abscess in the post-intervention phase (n = 9,12.9%). Ceftriaxone was the most commonly prescribed third- generation cephalosporin. It was given to 63 (89.9%) and 68 (97.1%) patients before and after intervention, respectively (Table II). There were no significant differences in length of stay (t = -1.874, p = 0.063), thirty-day readmission (X2 = 0.890, p = 0.822) and thirty-day mortality (X2 = 0.226, p = 0.698) between the two groups of patients.
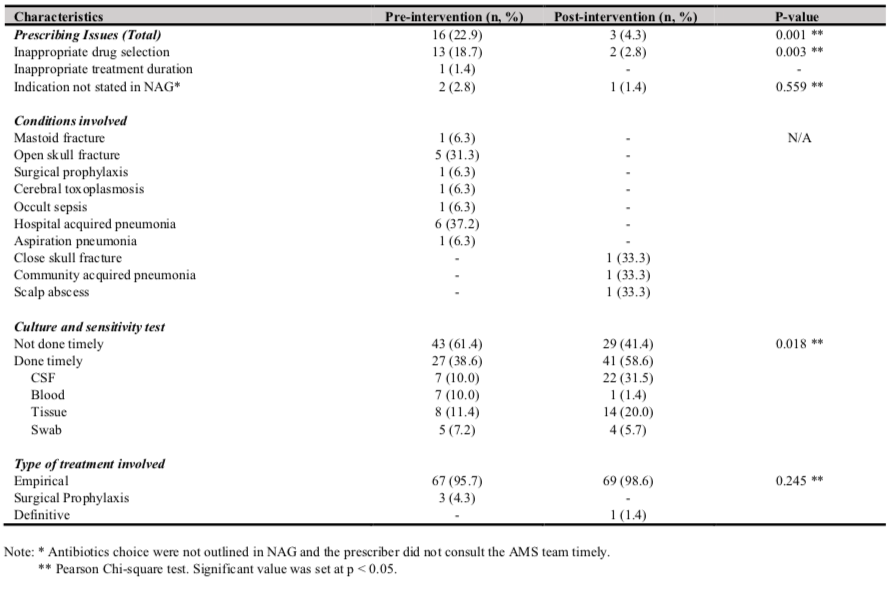
The proportion of cases with an appropriate use of third- generation cephalosporins had significantly increased from 77.1% (54 / 70) to 95.8% (67 / 70) following the intervention (X2 = 10.291, p = 0.001). Common issues detected in the pre- intervention phase included an inappropriate selection of antibiotics (n = 13 / 70, 18.7%) and an inappropriate treatment duration (n = 1 / 70, 1.4%). Of the 13 cases with an inappropriate antibiotic selection, five were open skull fracture and six were hospital-acquired pneumonia. After the intervention, an inappropriate selection of antibiotics was only observed in two cases (Table III). Additionally, there were three cases (2 before the intervention and 1 after the intervention) in which the use of antibiotics was not recommended in the NAG and the prescriber did not consult the AMS team beforehand.
The proportion of cases with C&S test performed timely also increased significantly from 38.6% (27 / 70) to 58.6% (41 / 70) following the intervention (X2 = 5.605, p = 0.018) (Table III.).
Discussion
This study shows that pharmacist-led audit-and-feedback intervention can serve as an effective approach to improve the appropriateness of third-generation cephalosporins prescribing in a hospital. It could also be used to promote the practice of performing the C&S tests timely, which are essential to guide the rational use of antibiotics in the ward. Meanwhile, the 30- day mortality, 30-day readmission and length of stay in hospital was similar in both groups of patients. In a previous study, it was found that a more comprehensive and intensive modules in multiple sessions could reduce the length of stay [18]. The single session educational intervention in this study may be inadequate to elicit significant change in clinical outcomes, and this may explain the similar mortality, readmission and length of stay among patients in the pre- and post-intervention cohorts.

As it would be expected, ceftriaxone emerged as the most commonly prescribed third-generation cephalosporin in the ward. In both the pre- and post-intervention phases, most patients received it as the empirical treatment for presumed bacterial meningitis. A previous study supported such a practice, suggesting that prompt treatment for presumptive meningitis with broad-spectrum antibiotics could lower the risk of mortality [19]. The latest evidence also recommends the use of either ceftriaxone or cefotaxime as the empirical treatment for the same condition [20]. It is noteworthy that we did not seek to change the existing practice but advocated for the use of antibiotics with a narrow spectrum of antimicrobial activities for other clinical conditions, such as intracranial trauma and open skull fracture, as recommended by the NAG (Table I).
It was also found that six patients with hospital-acquire pneumonia and one patient with aspiration pneumonia were treated with cefoperazone / sulbactam. However, the NAG recommends the use of amoxicillin/ clavulanate for early onset of both the conditions instead [20]. Such discrepancies were highlighted in the feedback session, and the appropriate drug selections for both the conditions were discussed. The prescribers adhered to this recommendation in the post- intervention phase, and no patient received cefoperazone / sulbactam for similar conditions. This suggests the prescribers have high level of acceptance towards evidence-based recommendations made by the AMS team.
There were also a few cases of basilar skull fracture complicated with CSF leak in both phases, for which antimicrobial treatment is not recommended by the NAG. However, the neurosurgical team raised their concern that the CSF leak could elevate the risk of meningitis. A consensus was reached in the feedback session that such a practice was acceptable. This shows a good example that the AMS team could play an integral role in providing timely and relevant advices when a condition is not captured by the NAG [15]. Similar conditions were also witnessed for cases of mastoid fracture, occult sepsis and close skull fracture.
In the pre-intervention phase, only 27 out of 70 (38.6%) patients had the C&S test performed timely. Ideally, the C&S test is to be performed before the initiation of antimicrobial treatment [22]. However, such a practice is often hindered by the complexity lumbar puncture (LP) procedure, as patients need to undergo a CT scan first and those with septic shock are unfit for the procedure [22]. Right after the feedback session, we observed a significant increase in the number of C&S tests performed timely. Previous study reported that physicians demonstrated distrust towards culture and sensitivity results, as it occasionally contradicted with patients’ clinical presentations [23]. Our educational audit-and-feedback session emphasized on the choice of narrow spectrum antibiotics to prevent antimicrobial resistance. This might have created awareness on the importance of timely C&S testing, led to increased C&S tests post-intervention.
This was the first local study evaluating the effectiveness of an audit-and-feedback intervention in improving third generation cephalosporins use among patients admitted in the neurosurgical ward. Nevertheless, as this was a single center study, the findings are not generalizable to other clinical settings. This was also a one-off audit, and thus the sustainability of the change in prescribing patterns could not be evaluated.
Conclusion
The pharmacist-led audit-feedback intervention was shown to be effective in improving the appropriateness of the third- generation cephalosporins use and timely C&S testing, indicating the antimicrobial stewardship strategy had produced a positive outcome. Further studies assessing the sustainability of the improvement are warranted.
Acknowledgement
There was no funding obtained for this work.
Conflict of Interest
This study has no conflict of interest. This research did not receive any specific grant from funding agencies in public, commercial or not-for-profit sectors.
References
- Buang SS, Haspani MS. Risk factors of neurosurgical site infections after a neurosurgical procedure: a prospective, observational study at Hospital Kuala Lumpur. Medical Journal of Malaysia. 2012; 67(4): 393-86.
- Guruja MP, Sarah A, Samaga L, Joshi H, Nair S, Shastry CS. Cephalosporin utilization evaluation in a university teaching hospital: a prospective study. Journal of Drug Delivery and Therapeutics. 2013; 3(2): 83-87. https://doi.org/10.22270/jddt.v3i2.399
- Mc Gowan JE, Tenover FC. Control of antimicrobial resistance in the health care system. infectious disease clinics of North America. 1997; 11(2):297–311. https://doi.org/10.1016/s0891-5520(05)70357-3
- Park SH. Third generation cephalosporin resistance in gram-negative bacteria in the community: a growing public health concern. Korean Journal of International Medicine. 2014; 29(1): 27-30. https://doi.org/10.3904/kjim.2014.29.1.27
- Abou-Shaaban, Ali AA, Rao PG, Majid A. Drug utilization review of cephalosporins in a secondary care hospital in United Arab Emirates. International Journal of Clinical Pharmacy. 2016; 38(6): 1367-1371. https://doi.org/10.1007/s11096-016-0392-4
- Naveen V, Siddiq A, Chandana G. A study of drug utilization pattern of cephalosporins in general medicine and surgical inpatient department. International Journal of Current Pharmaceutical Research. 2018; 10(3): 33-36. https://doi.org/10.22159/ijcpr.2018v10i3.27225
- Sileshi, A., Tenna, A., Feyissa, M., & Shibeshi, W. (2016). Evaluation of ceftriaxone utilization in medical and emergency wards of Tikur Anbessa specialized hospital: A prospective cross-sectional study. BMC Pharmacology & Toxicology, 17. https://doi.org/10.1186/s40360-016-0057-x
- Opanga SA, Nimrod JA, Faith AO, Kimani AM. Patterns of antimicrobial use in neurosurgical ward of Kenyatta National Hospital. African Journal of Pharmacology and Therapeutics. 2016; 5(4): 241-246
- Sharma MS, Suri A, Chandra SP, Kale SS, Kapil A, Sharma BS, Mahapatra AK. Cost and usage pattern of antibiotics in a tertiary care of neurosurgical unit. Indian Journal of Neurosurgery. 2012; 1(1): 41- 7. https://doi.org/10.4103/2277-9167.94370
- Malaysian Action Plan on Antimicrobial Resistance, 2017-2021. Ministry of Health Malaysia and Ministry of Agriculture and Agro- based Industry Malaysia. https://www.moh.gov.my/moh/resources/Penerbitan/Garis%20Panduan/Garis%20panduan%20Umum%20(Awam)/National_Action_Plan_-_FINAL_29_june.pdf
- Lim MK, Lai PS, Ponnampalavanar SS, Syed Omar SF, Taib NA, Yusof MY, Italiano CM, Kong DC, Kamarulzaman A. Antibiotics in surgical wards: use or misuse? A newly industrialized country’s perspective. J Infect Dev Ctries. 2015 Nov 30;9(11):1264-71. https://doi.org/10.3855/jidc.6731
- Gillani, S. W., Sulaiman, A. S., & Nejad, F. B. (2010). Inpatient care and microbial surveillance during year 2007-2008; retrospective evaluation of hospital-acquired pneumonia (HAP) in General Hospital Pulau Pinang, Malaysia. International Journal of Food Safety, Nutrition and Public Health, 3(1), 27–32. https://doi.org/10.1504/IJFSNPH.2010.032032
- Parulekar L, Soman R, Singhal T, Rodrigues C, Dastur FD, et al. How good is compliance with surgical antibiotic prophylaxis guidelines in a tertiary care private hospital in India? A prospective study. Indian Journal of Surgery .2009; 71: 15-18. https://doi.org/10.1007/s12262-009-0004-9
- Ministry of Health Malaysia. Protocol on antimicrobial stewardship program in healthcare facilities. 2014. https://www.pharmacy.gov.my/v2/en/documents/protocol- antimicrobial-stewardship-program-healthcare-facilities.html
- Høgli JU, Garcia BH, Skjold F, Skogen V, Småbrekke L. An audit- and-feedback intervention study increased adherence to antibiotic prescribing guidelines at a Norwegian hospital. BMC Infect Dis. 2016 Feb 27;16:96. https://doi.org/10.1186/s12879-016-1426-1
- Ivers, N., Jamtvedt, G., Flottorp, S., Young, J. M., Odgaard‐Jensen, J., French, S. D., O’Brien, M. A., Johansen, M., Grimshaw, J., & Oxman, A. D. Audit-and-feedback: Effects on professional practice and healthcare outcomes. Cochrane Database of Systematic Reviews. 2012 Jun 13;(6)CD000259. https://doi.org/10.1002/14651858.CD000259.pub3
- McCambridge J, Witton J, Elbourne DR. Systematic review of the Hawthorne effect: new concepts are needed to study research participation effects. J Clin Epidemiol. 2014 Mar; 67(3):267-77. https://doi.org/10.1016/j.jclinepi.2013.08.015
- Manheim LM, Feinglass J, Hughes R, Martin GJ, Conrad K, Hughes EF. Training house officers to be cost conscious. Effects of an educational intervention on charges and length of stay. Med Care. 1990 Jan;28(1):29-42. https://doi.org/10.1097/00005650-199001000-00005
- Proulx N, Frechette D, Toye B, Chan J, Kravcik S. Delays in the administration of antibiotics are associated with mortality from adult acute bacterial meningitis. QJM 2005; 98: 291–8. https://doi.org/10.1093/qjmed/hci047
- Ministry of Health Malaysia, National Antimicrobial Guidelines (2019). https://www.pharmacy.gov.my/v2/sites/default/files/documen t-upload/national-antimicrobial-guideline-2019-full-version-3rd- edition.pdf
- Young, N., & Thomas, M. (2018). Meningitis in adults: Diagnosis and management. Internal Medicine Journal, 48(11), 1294–1307. https://doi.org/10.1111/imj.14102
- McGill F, Heyderman RS, Michael BD, Defres S, Beeching NJ, Borrow R et al. The UK joint specialist societies guideline on the diagnosis and management of acute meningitis and meningococcal sepsis in immunocompetent adults. J Infect 2016; 72: 405–38. https://doi.org/10.1016/j.jinf.2016.01.007
- Rolfe, R., Kwobah, C., Muro, F. et al. Barriers to implementing antimicrobial stewardship programs in three low- and middle-income country tertiary care settings: findings from a multi-site qualitative study. Antimicrob Resist Infect Control 10, 60 (2021). https://doi.org/10.1186/s13756-021-00929-4
Please cite this article as:
Rou Wei Tan, Chee Tao Chang, Kah Shuen Thong, Joo Thye Cheng, Huan Keat Chan and Meng Fei Cheah, Effectiveness of Pharmacist-Led Audit-and-Feedback Intervention in Promoting Appropriate Third-Generation Cephalosporin Use at a Tertiary Public Hospital in Malaysia. Malaysian Journal of Pharmacy (MJP). 2021;2(7):7-12. https://mjpharm.org/effectiveness-of-pharmacist-led-audit-and-feedback-intervention-in-promoting-appropriate-third-generation-cephalosporin-use-at-a-tertiary-public-hospital-in-malaysia/